Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) is a rare autoimmune disease characterized by skin and organ fibrosis and vasculopathy. The Very Early Diagnosis of SSc (VEDOSS) project (Bellando-Randone S, et al. Lancet Rheum. 2021. 3(12); E834-E843) recently identified the value of predefined red flag symptoms or signs as a stratification tool for the risk of fulfilling the 2013 ACR/EULAR classification criteria for SSc. However, to date, an analysis of symptoms and signs prior to an SSc diagnosis has not been performed. Understanding pre-diagnostic patient pathways can help identify other major signs preceding a diagnosis, identify the burden of very early disease in patients with scleroderma and the potential barriers to early intervention. This study aimed to categorize temporal disease patterns leading to the initial diagnosis of SSc using US and Japanese health insurance claims data.
Methods: Patients with a diagnosis of SSc were identified from two claims databases (Optum® Clinformatics® and JMDC for the US and Japan, respectively). Patients with at least two concordant medical claims associated with SSc (International Classification of Diseases [ICD]-9 710.1, 517.2) on different dates within a 1-year period and who were ≥18 years old at the time of first SSc diagnosis were included. In the US, records were gathered from January 1, 2007 to September 30, 2015, and in Japan from January 1, 2005 to November 30, 2019. ICD codes of the differential diagnostic claims in the 3 years before SSc diagnosis were recorded. Network analysis and sequential pattern mining were used to identify and visualize temporal disease patterns prior to the diagnosis of SSc.
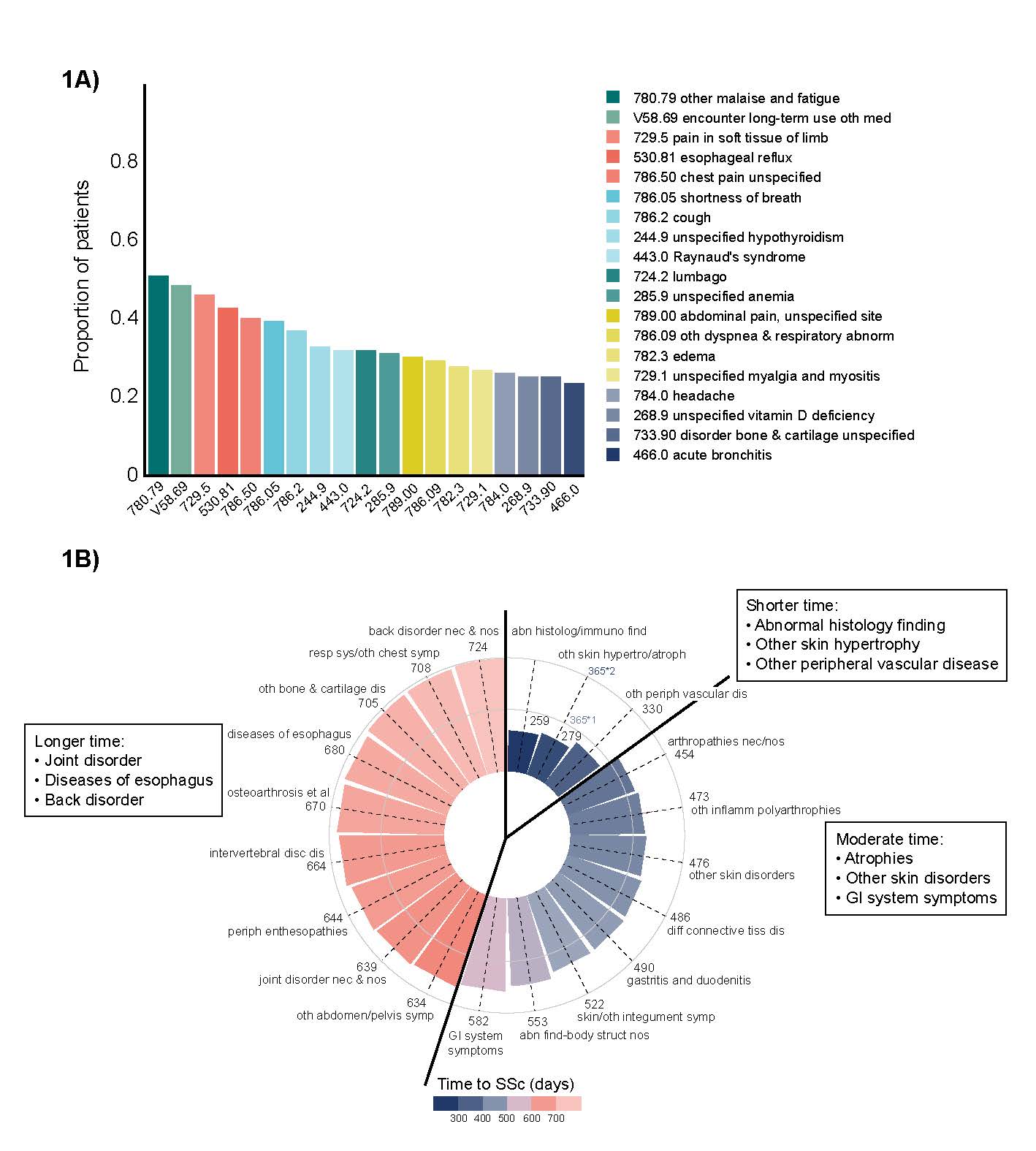
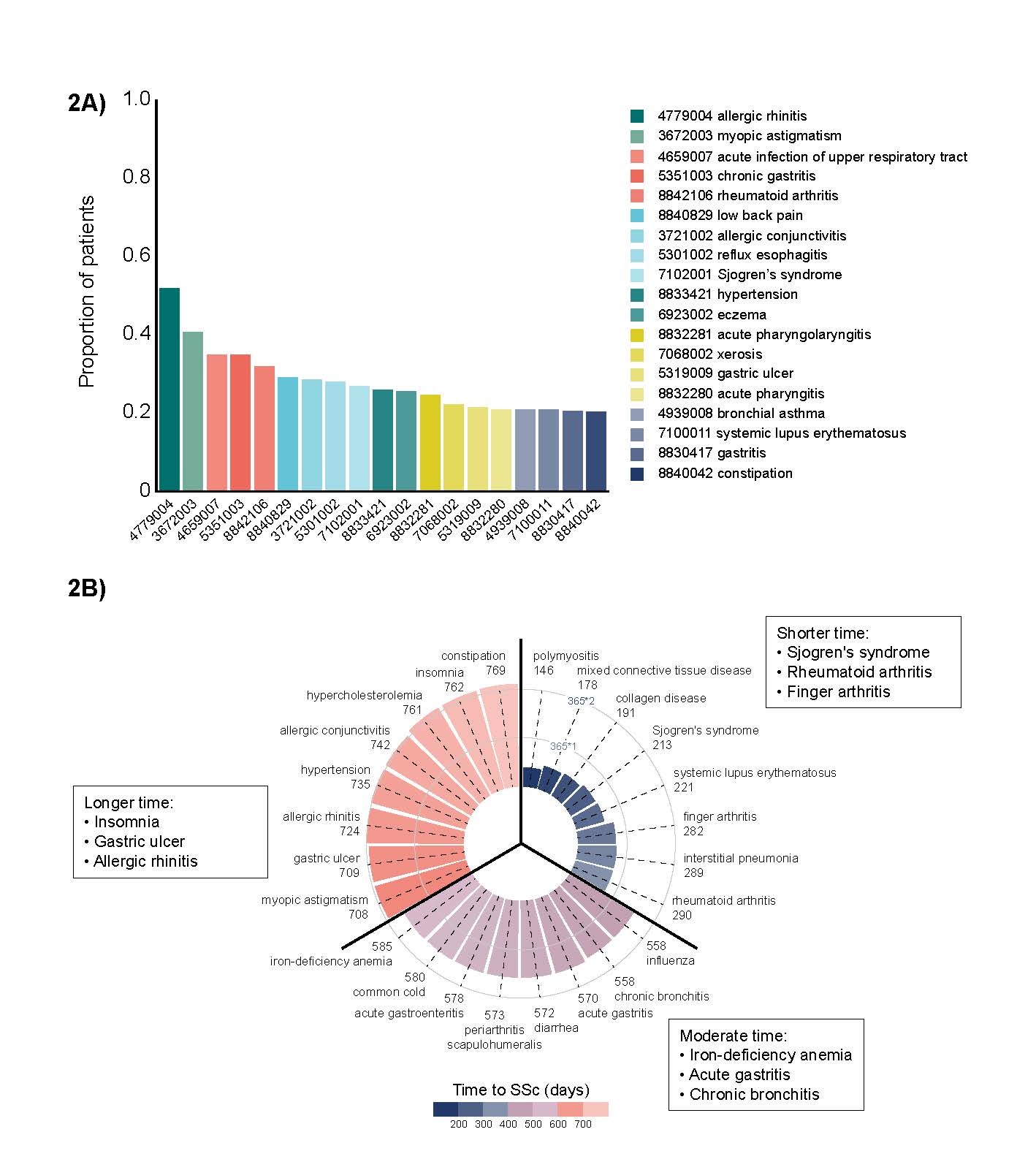
Results: In total, 2550 patients with continuous insurance history for ≥3 years prior to their SSc diagnosis (1765 from the US and 785 from Japan) were analyzed. Mean age at first SSc diagnosis was 61 and 51 years for the US and Japan, respectively. Approximately 80% of patients were female. In the US, the five most common diagnoses prior to SSc were related to fatigue, pain or discomfort, followed by esophageal reflux and chest pain in Japan, the most common diagnoses included upper respiratory infection, gastritis and rheumatoid arthritis (Figures 1a & 2a). In both countries, the mean time to diagnosis was shorter when the presenting complaint was Raynaud’s-related (428 days in the USA and 327 days in Japan), whereas it was almost double this when the complaint was more related to joint pain, fatigue or GI symptoms (Figures 1b & 2b).
Conclusion: Collectively, within the limitations of analyzing data from insurance claims and ICD codes, these real-world data showing a range of diagnoses prior to SSc help to identify the health burden leading to a diagnosis of SSc. These findings suggest that symptoms not directly related to Raynaud’s or skin manifestations such as upper GI involvement and joint pain may not be recognized as early signs of SSc. Further deconvolution of the frequency and temporal distribution of symptoms that patients commonly present with prior to being diagnosed with SSc could help identify other “red flags” that physicians should consider when triggering a diagnostic workup for SSc, ultimately improving early detection and long-term outcomes.
To cite this abstract in AMA style:
Del Galdo F, Tian Y, Di Donato S, Ehlers M. The Patient Journey to a First Diagnosis of Systemic Sclerosis: Temporal Disease Pattern Identification Using Machine Learning and Data Mining Among US and Japanese Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-patient-journey-to-a-first-diagnosis-of-systemic-sclerosis-temporal-disease-pattern-identification-using-machine-learning-and-data-mining-among-us-and-japanese-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-patient-journey-to-a-first-diagnosis-of-systemic-sclerosis-temporal-disease-pattern-identification-using-machine-learning-and-data-mining-among-us-and-japanese-patients/