Session Information
Date: Tuesday, November 14, 2023
Title: (1945–1972) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial Lung Disease (ILD), prevalent in Idiopathic Inflammatory Myositis (IIM) patients, significantly impacts prognosis. Certain myositis-specific antibodies, including anti-MDA5 and anti-aminoacyl-tRNA synthetases (ARS), are linked to increased ILD incidence, while other myositis antibodies were rarely discussed. Recent evidence suggests survival rates among Interstitial Pneumonitis with Autoimmune Feature (IPAF) patients harboring myositis specific antibodies (MSA) parallel those with IIM-ILD [1]. Our study aims to investigate the pulmonary involvement in IIM and IPAF patients, emphasizing the role of diverse myositis antibodies, within a single center cohort.
Methods: From Jan. 2010 to Dec. 2022, patients diagnosed with IIM who underwent myositis antibody testing were identified in a Taiwan medical center. Additionally, 49 patients diagnosed with IPAF per the 2015 ERS statement with positive myositis antibody result were also enrolled for analysis.[2] The diagnosis of ILD was confirmed by a HRCT finding. The myositis antibodies were determined through line-blot multiplex assay (Autoimmune Inflammatory Myopathies 16 Ag, Euroimmun, Lu ̈ beck, Germany), encompassing 16 autoantigens.
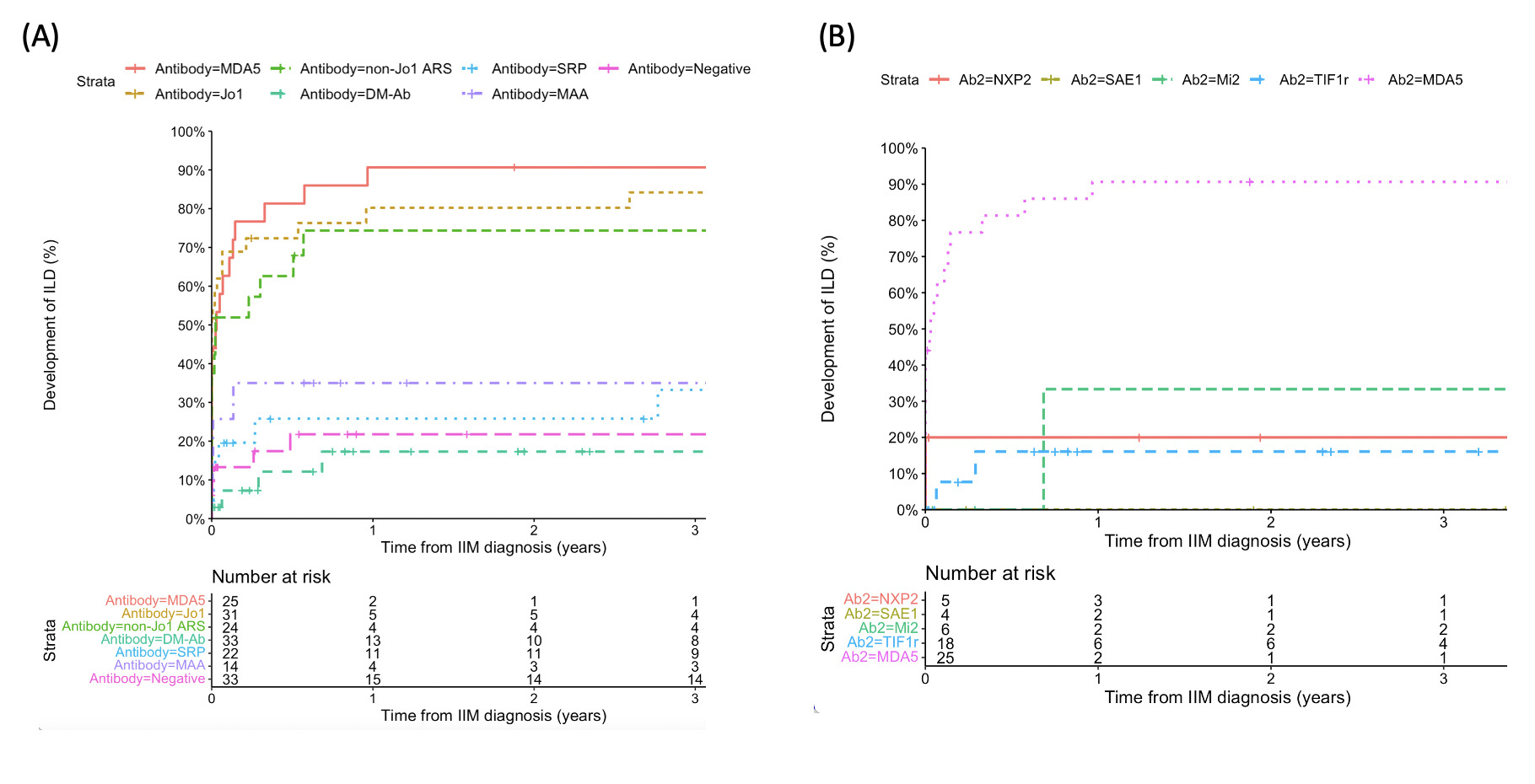
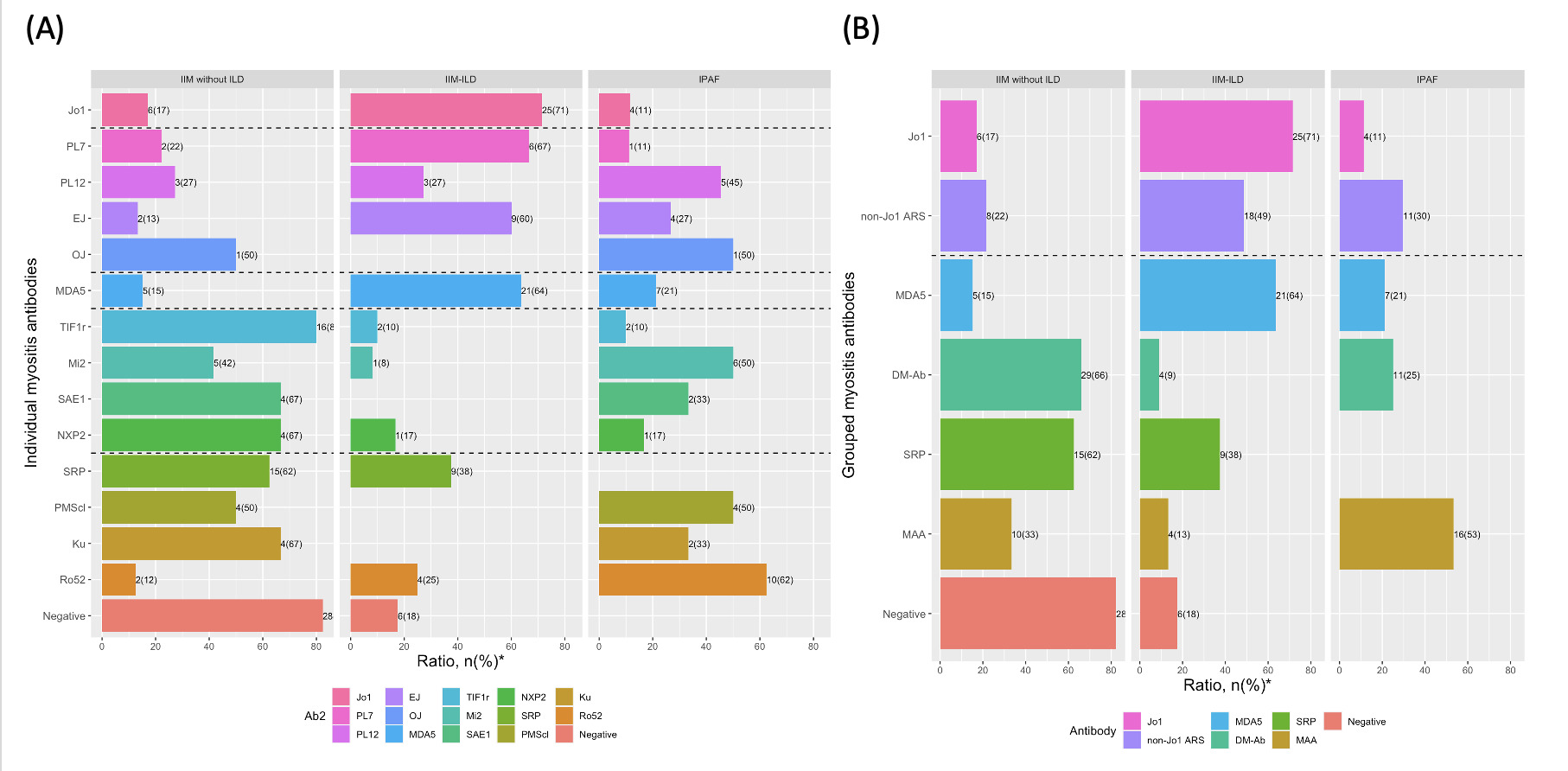
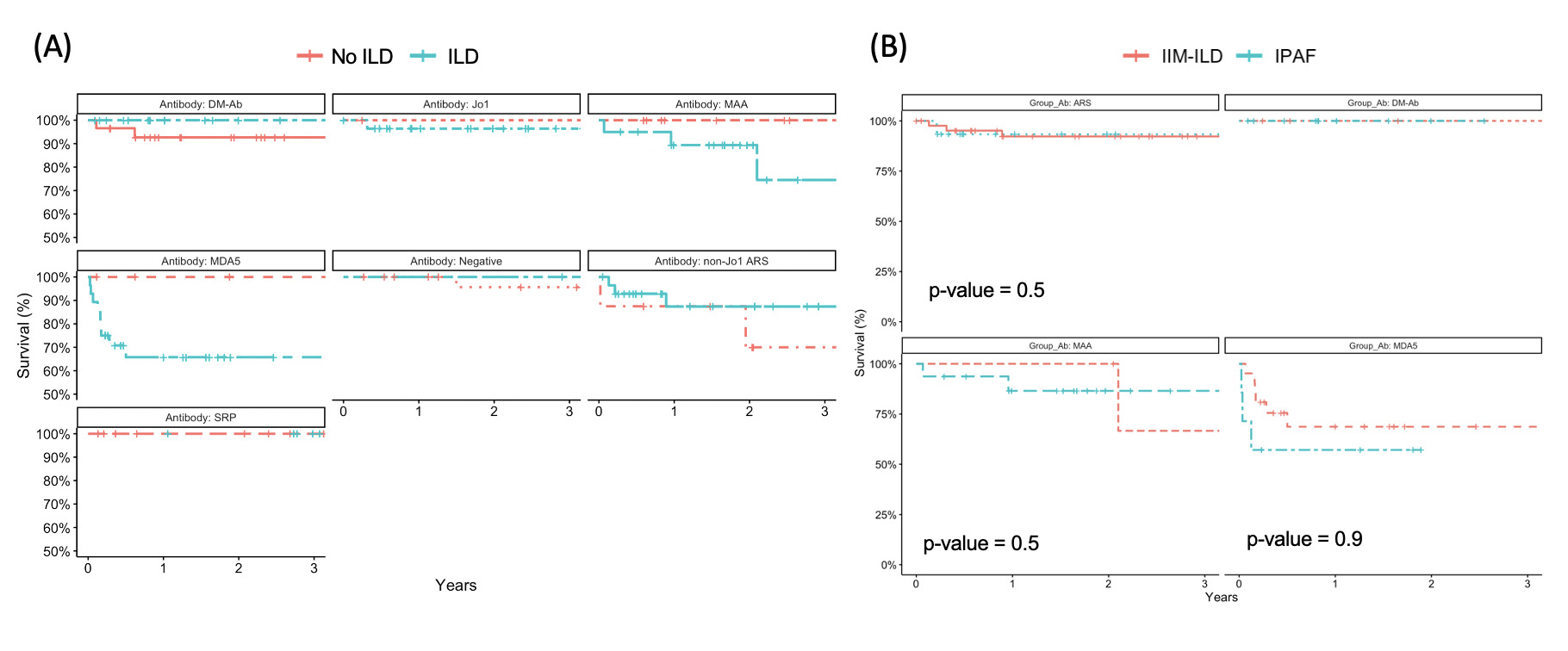
Results: 118 IIM patients (mean age 52, 75% female) and 49 IPAF patients (mean age 67, 49% female) were enrolled. The anti-MDA5 and ARS were significantly associated with ILD development, exhibiting the 3-year incidence exceeding 70%, with most cases presenting within the first year post-diagnosis. Approximately 40% patients with anti-SRP ultimately developed ILD (Figure 1A). In patients with DM-specific antibodies (TIF1r, Mi2, SAE1, NXP2, MDA5, as defined by ENMC 2020 consensus) except for anti-MDA5, most remained ILD-free 3 years post-diagnosis (Figure 1B). A non-negligible fraction of patients with anti-MDA5, anti-ARS, and dermatomyositis-specific antibodies presented with IPAF instead of IIM or ASS (Figure 2). However, the correlation between ILD and poor prognosis only exist for patients with anti-MDA5 and MAA (Figure 3A). Furthermore, the 3-year survival rate for IIM-ILD and IPAF patients with anti-MDA5 (68% vs 57%, p=0.9) , anti-ARS (92% vs 93%, p=0.5) and DM-specific antibodies (100% vs 100%) were similar (Figure 3B).
Conclusion: Anti-MDA5 and ARS antibodies demonstrated a strong correlation with ILD development, and prognosis was consistent among IIM-ILD and IPAF patients. Other dermatomyositis-specific antibodies and anti-SRP were also associated with ILD development, albeit to a lesser extent, and the onset of ILD did not correlate with a poorer prognosis.
To cite this abstract in AMA style:
Lan T, Lee T, Lin K, Kao J, Cheng C, Lu C, Shen C, Li K, Hsieh S. The Influence of Specific Myositis Antibodies on the Development of Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-influence-of-specific-myositis-antibodies-on-the-development-of-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-influence-of-specific-myositis-antibodies-on-the-development-of-interstitial-lung-disease/