Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Upon transitioning from pediatric to adult care, many patients with JIA are labeled as having RA, despite the two diagnoses being distinct in care and treatment. We investigated differences between adult patients with JIA and those with RA, and between adult patients with JIA who retain their diagnosis and those who are reclassified to RA, in a 20-year observational study.
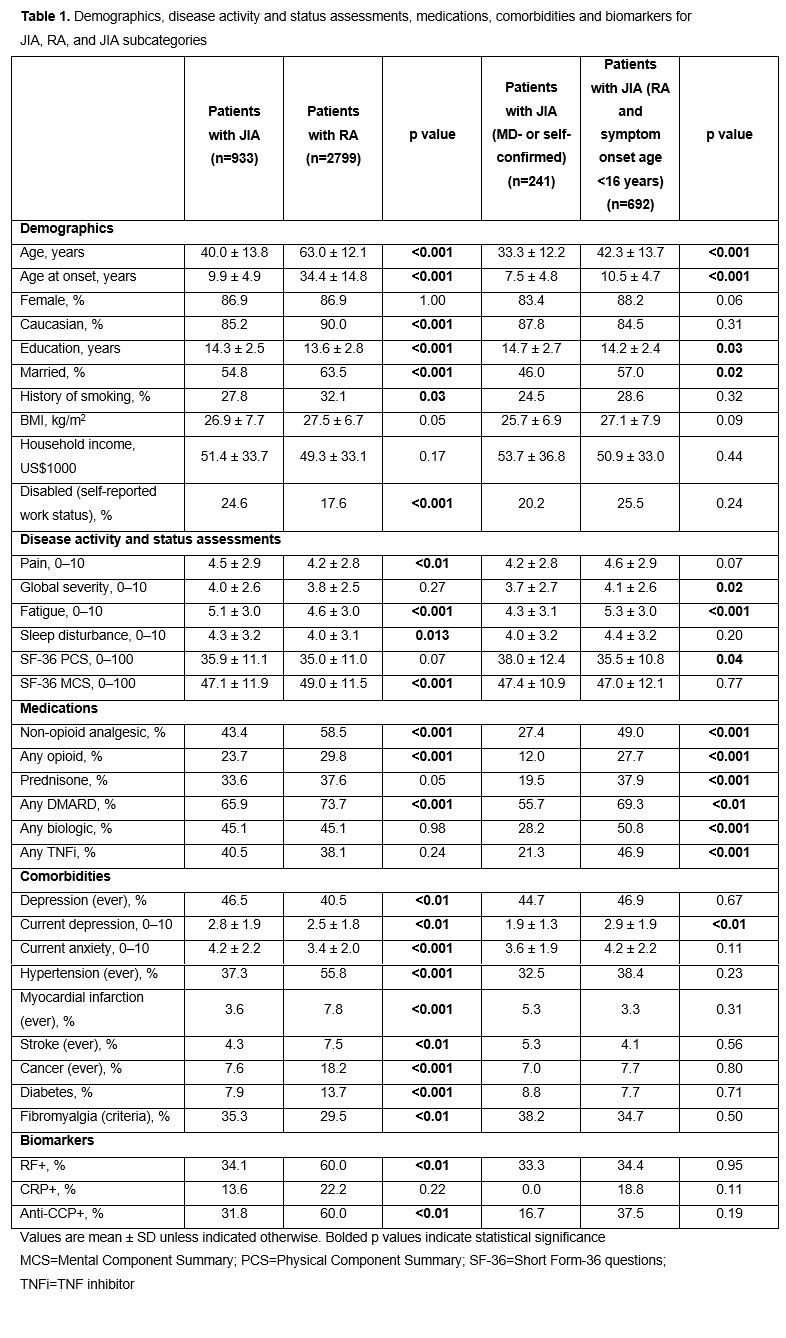
Methods: Patients enrolled in a large, US-wide longitudinal study of rheumatic disease outcomes from 1998 to 2018 were eligible. Random observations from adults with JIA were analyzed descriptively and matched 1:3 with patients with RA. Matching was performed based on sex, calendar year of observation, and calendar year of diagnosis to produce matching disease duration and treatment era comparisons. Demographics, disease activity and status assessments, medications, co-morbidities and biomarkers were compared using t-tests and Chi-square tests. Logistic regression models for JIA versus RA diagnosis and for JIA diagnosis type were generated using backward elimination at p< 0.05.
Results: In the JIA cohort (n=933), 25.8% of patients had physician-confirmed or self-reported JIA and 74.2% had physician-confirmed RA with symptom onset prior to age 16 (Table 1). Nearly all (92.3%) patients with JIA who were given an RA diagnosis had symptoms prior to the terminology change from juvenile RA to a JIA diagnosis, versus 57.7% of other patients with JIA. Biomarkers were identified in a subset of patients: 38.6% of all patients with JIA (n=44) and 68.9% of matched patients with RA (n=135) were RF+ and/or anti-CCP+ (data not shown). After addressing confounding in logistic regression models, several parameters were associated with JIA (vs RA) diagnosis, including younger age, lower pain and abatacept use, and higher fatigue among others (Figure 1A). In comparing the diagnosis type within the JIA cohort, older age, older age at symptom onset, lower Short Form-36 physical component summary score, symptom onset prior to the JIA terminology change and higher infliximab use were associated with labeling patients with RA in adulthood (Figure 1B).
Conclusion: Matched adults with JIA or RA had important differences in patient-reported outcomes, medication use and co-morbidities. Diagnoses given to adults with JIA have an important impact on their treatments, as reclassification to RA leads to differences in those treatments, particularly with use of infliximab.
Writing support: Katerina Kumpan at Caudex; funding: Bristol-Myers Squibb
*at the time of the analysis
To cite this abstract in AMA style:
Wipfler K, Pedro S, Shaw Y, Schumacher R, Simon T, Dominique A, Reinhardt A, Michaud K. The Importance of Diagnosis: Clinical Distinctions Between Adult JIA and RA, and a Characterization of Patients with JIA Reclassified as RA in Adulthood [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-importance-of-diagnosis-clinical-distinctions-between-adult-jia-and-ra-and-a-characterization-of-patients-with-jia-reclassified-as-ra-in-adulthood/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-importance-of-diagnosis-clinical-distinctions-between-adult-jia-and-ra-and-a-characterization-of-patients-with-jia-reclassified-as-ra-in-adulthood/