Session Information
Session Type: Abstract Session
Session Time: 11:00AM-11:15AM
Background/Purpose: Systemic lupus erythematosus (SLE) has the 6th highest hospital readmission rate of all US chronic diseases with significant health disparities and costs. Transitional care management with higher reimbursement for post-discharge care within 14 days has been shown to decrease 30-day hospital readmissions in other chronic diseases. However, the impact of timely follow-up care (within 14 days) on readmission has not been evaluated among SLE patients. Our objectives were to (1) examine predictors of timely post-discharge follow-up and (2) compare all-cause 30-day readmissions after hospitalization with and without timely ambulatory follow-up among SLE patients.
Methods: We conducted a retrospective cohort study using a 20% random sample of all US Medicare hospitalizations in 2014. Hospitalized patients in the study had an SLE diagnosis code, age ≥18 years, alive at discharge, discharged to home, and not receiving hospice. Baseline characteristics of patients with inpatient stays with and without follow-up with a primary care provider or rheumatologist within 14 days of index hospital discharge were compared. Multivariate general estimating equation (GEE) models clustered by patient were used to determine the predictors and the effects of timely follow-up on 30-day rehospitalization risk.
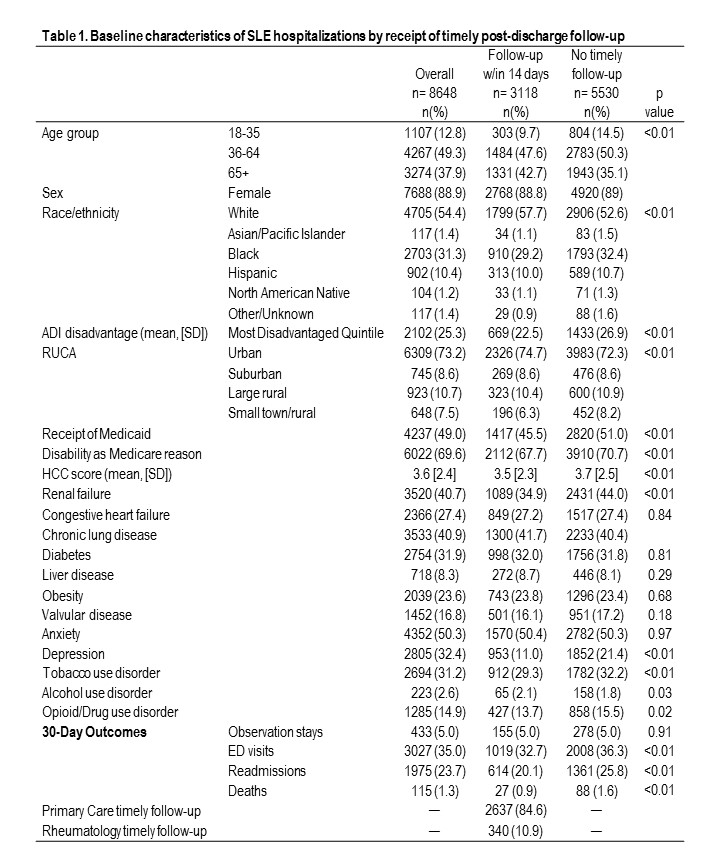
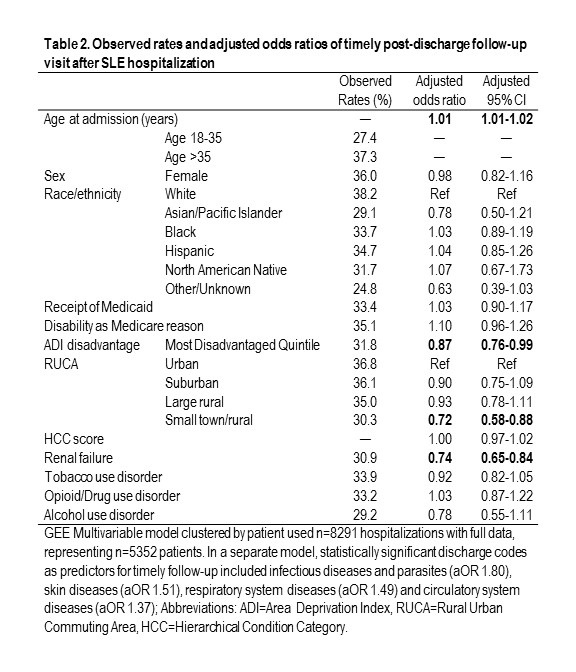
Results: Compared to SLE admissions with timely (within 14 days) post-hospitalization follow-up (n=3118, 36%), those without timely follow-up (n=5530, 64%) were more likely to be younger, non-White, and living in the most disadvantaged neighborhoods (Table 1). Patients without timely follow-up were more likely to have comorbidities such as renal failure, depression, and tobacco, drug, or opioid use disorders. Observed thirty-day readmission rates were higher among those without timely follow-up (26% vs 20%), and only 11% of follow-up within 14 days was with rheumatology. Young adults had 10% lower timely follow-up (27 vs 37%) and 15% higher readmissions (37 vs 22%; Tables 2 & 3). Multivariable predictors of timely follow-up showed higher odds per year of age (aOR 1.01 (1.01,1.02); Table 2), but lower odds for those with renal failure (aOR 0.74 (0.65,0.84)), and those residing in the most disadvantaged neighborhoods (aOR 0.87 (0.76,0.99)) and rural areas (aOR 0.72 (0.58,0.88)). Timely post-discharge follow-up predicted 21% lower odds of readmission (aOR 0.79 (0.70,0.89); Table 3). Unlike younger age, race/ethnicity, rurality, and neighborhood disadvantage did not predict readmission risk after considering timely follow-up.
Conclusion: Hospitalized Medicare beneficiaries with SLE were 20% less likely to be readmitted within 30 days if they received post discharge follow-up within 14 days with either rheumatology or primary care, even after adjusting for comorbidities. Adjusted risk factors for lack of timely follow-up care included younger age, living in the most disadvantaged neighborhoods or in a rural area, and renal failure. To overcome limitations in this study our next analysis will explore whether immortal time bias influences outcomes. Other future studies should investigate targeted interventions to increase timely post-discharge follow-up care to reduce SLE readmissions and health disparities.
To cite this abstract in AMA style:
Schletzbaum M, Sweet N, Powell W, Gilmore Bykovskyi A, Kaiksow F, Sheehy A, Kind A, Bartels C. The Impact of Timely Post-Discharge Follow-up on Readmission Risk Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-timely-post-discharge-follow-up-on-readmission-risk-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-timely-post-discharge-follow-up-on-readmission-risk-among-patients-with-systemic-lupus-erythematosus/