Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease in children with uveitis as the most common extra-articular manifestation. Uveitis can lead to sight-threatening complications and vision loss. While outcomes are influenced by disease phenotype and clinical risk factors, social determinants of health may significantly impact disease burden. The CDC’s Social Vulnerability Index (SVI) is a composite measure of socioeconomic and demographic stressors and has not previously been applied to pediatric uveitis. This study investigates whether higher SVI is associated with delayed diagnosis, worse quality of life (QoL), and poorer clinical outcomes in affected children.
Methods: This retrospective single-center study included children diagnosed with JIA without uveitis (JIA-no-U), JIA-associated uveitis (JIA-U), and uveitis-only (Uveitis) from the Longitudinal Outcomes of Childhood Uveitis Study (LOCUS) registry. For SVI analyses, JIA-U and uveitis-only were combined as a single group (Uveitis). SVI scores (0 = low, 1 = high) were derived from addresses in the Electronic Medical Record using deGAUSS software and divided into quartiles (Q1–Q4). Analyses compared Q1 (low) and Q4 (high). Variables included demographics, age at diagnosis, time to systemic immunosuppression, and Pediatric QoL Inventory (PedsQL-Child Total) scores, an age-appropriate outcome measure. Analyses used t-tests and ANOVA. Some dates were recorded only by year, limiting precision.
Results: Of 509 patients, 357 had JIA-no-U, 127 JIA-U, and 25 uveitis-only (Table 1). Compared to JIA-only, JIA-U patients were more likely to be ANA-positive (49.6% vs 26.3%, p< 0.001) and female (78.0% vs 64.4%, p< 0.0001).SVI Q4 was linked to later mean uveitis onset (Q4: 6.8 vs Q1: 4.1 yrs; p=0.0004) but not JIA-only onset (Q4: 5.8 vs Q1: 4.5 yrs; p=0.1347) (Figure 1A). Time to systemic immunosuppression showed opposite SVI associations (Figure 1B): in JIA-only, systemic treatment for Q4 was delayed (52.2 vs 11.6 weeks; p=0.000); for the Uveitis group, Q4 had shorter time to systemic treatment (27.8 vs 49.3 weeks; p=0.000). For QoL, Uveitis patients in Q4 reported significantly worse PedsQL scores (Q4: ~40 vs Q1: ~75; p< 0.01). In JIA-only, scores did not differ significantly (Q4: ~79 vs Q1: ~82; p=0.4815) (Figure 2).
Conclusion: Social vulnerability significantly impacts key clinical outcomes and QOL in pediatric uveitis. Higher SVI patients with uveitis received systemic therapy more quickly, perhaps indicating severity at onset and rapid need for treatment escalation to prevent vision loss. Further, they are at risk for delayed uveitis diagnosis and poorer QOL. The SVI may serve as a valuable risk stratification tool to guide early intervention and targeted care coordination in at-risk children. Further study is warranted to evaluate subtype-specific mechanisms and treatment adherence patterns.
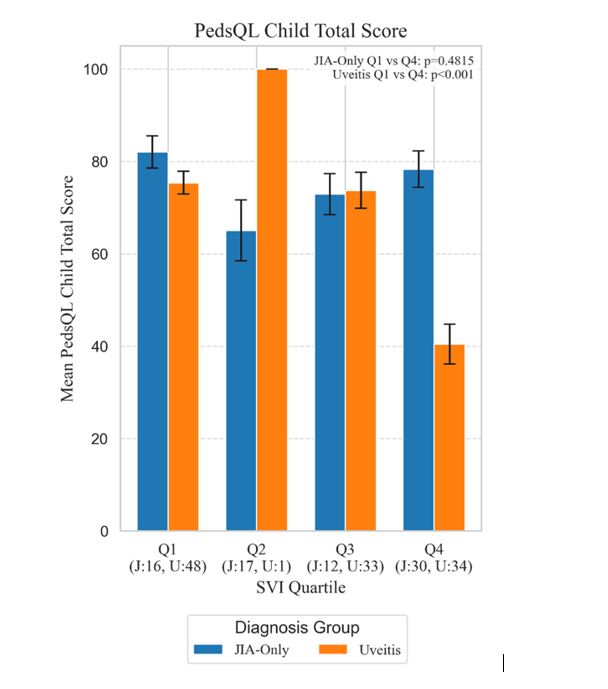 Table 1: Baseline Demographics and Clinical Characteristics of JIA-Only and Uveitis Cohorts.
Table 1: Baseline Demographics and Clinical Characteristics of JIA-Only and Uveitis Cohorts.
.jpg) Figure 1. Impact of Social Vulnerability Index (SVI Q1=Low, Q4=High) on Disease Onset and Treatment Timing. (A) Mean age at JIA-Only and Uveitis onset by SVI Quartile. (B) Mean time to systemic immunosuppression in JIA-only and Uveitis patients by SVI Quartile. *P-values shown for comparisons.
Figure 1. Impact of Social Vulnerability Index (SVI Q1=Low, Q4=High) on Disease Onset and Treatment Timing. (A) Mean age at JIA-Only and Uveitis onset by SVI Quartile. (B) Mean time to systemic immunosuppression in JIA-only and Uveitis patients by SVI Quartile. *P-values shown for comparisons.
.jpg) Figure 2. Association of Social Vulnerability Index (SVI Q1=Low, Q4=High) with mean PedsQL Child Total Score. Higher scores indicate better QoL. *P-values shown for comparisons.
Figure 2. Association of Social Vulnerability Index (SVI Q1=Low, Q4=High) with mean PedsQL Child Total Score. Higher scores indicate better QoL. *P-values shown for comparisons.
To cite this abstract in AMA style:
Aundhia M, Rajdeo P, Wagner M, Duell A, Quinlan-Waters M, Miraldi Utz V, Angeles-Han S. The Impact of Social Vulnerability Index Scores in Pediatric Uveitis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-social-vulnerability-index-scores-in-pediatric-uveitis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-social-vulnerability-index-scores-in-pediatric-uveitis/
