Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Session Type: Poster Breakout Session
Session Time: 4:30PM-5:00PM
Background/Purpose: Youth with systemic lupus erythematosus (SLE) experience significant health care burden and high rates of psychiatric disorders. Optimizing medication adherence is critical for preventing organ damage and death. We examined the effect of psychiatric disorders on hydroxychloroquine adherence rates, and tested whether the effect differs by psychiatric treatment.
Methods: We identified incident hydroxychloroquine users among youth with SLE (ages 10-24 years) using U.S. commercial insurance claims in Optum’s de-identified Clinformatics® Data Mart (2000-2016). The index prescription was the first pharmacy claim for hydroxychloroquine with none in the preceding year. Adherence was estimated by medication possession ratios (MPR), defined as days supply over a fixed 365-day interval after the index prescription, excluding hospital days. The primary exposure was any psychiatric diagnosis in the year preceding the index prescription, further categorized into depression, anxiety, adjustment or other psychiatric disorders. We used two-sample t-tests to compare MPRs among youth with or without psychiatric diagnoses. Multivariable linear regression with backward selection was used to estimate the effect of psychiatric diagnoses, adjusted for demographic characteristics and proxies for disease severity. We tested for interactions between psychiatric diagnoses and psychiatric treatment, including psychotropic medication use and psychotherapy.
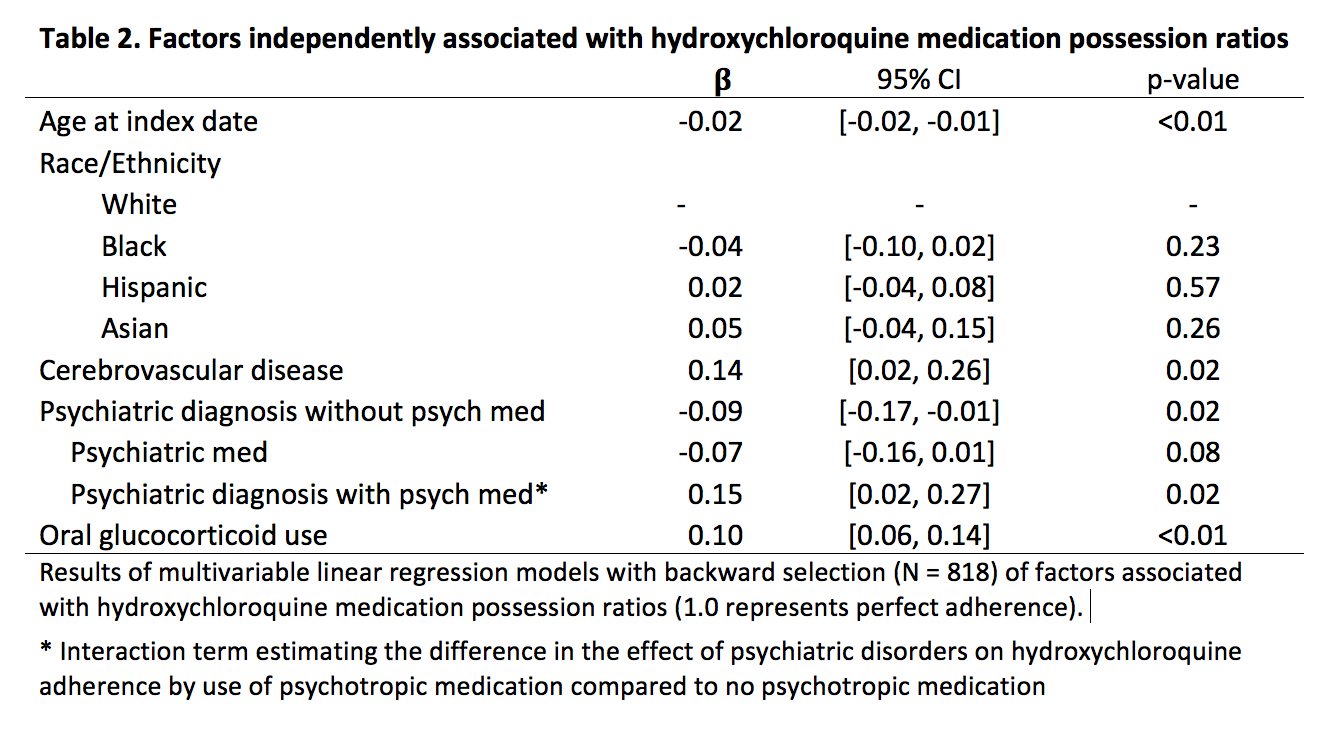
Results: There were 873 incident hydroxychloroquine users with a mean age of 19.2 (±3.3). 20% of subjects had a psychiatric diagnosis, of which depression was most common (Table 1). There were no unadjusted differences in mean MPRs among those with or without psychiatric diagnoses (mean 0.54 (±0.3) vs 0.58 (±0.3), p=0.16). In the adjusted analysis, there was also no average effect of having any psychiatric diagnosis on MPR (b -0.04, p=0.15). Only adjustment disorders were independently associated with a decrease in MPR (-0.13, 95% CI [-0.24, -0.01], p=0.03). However, there was a significant crossover interaction, in which psychiatric diagnoses had opposite effects on adherence depending on psychotropic medication use (Fig. 1). The presence of any psychiatric diagnosis without psychotropic medications was associated with a 0.09 decrease in MPR compared with no psychiatric diagnosis (95% CI [-0.17, -0.01], p=0.02). However, among youth with a psychiatric diagnosis, psychotropic medication use was associated with a 0.15 increase in MPR (p=0.02 for interaction) (Table 2). Similar patterns were seen for depression and anxiety, but not for adjustment disorders (Fig. 1). Among youth with anxiety disorders, psychotherapy was also associated with a 0.23 increase in MPR compared to no psychotherapy (p< 0.01 for interaction).
Conclusion: The impact of psychiatric disorders on medication adherence differed significantly by whether youth were taking psychotropic medications or receiving psychotherapy, which may indicate ongoing psychiatric treatment. This suggests that improving recognition and treatment of psychiatric conditions may increase medication adherence in youth with SLE.
To cite this abstract in AMA style:
Chang J, Davis A, Klein-Gitelman M, Cidav Z, Mandell D, Knight A. The Impact of Psychiatric Diagnosis and Treatment on Medication Adherence in Youth with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/the-impact-of-psychiatric-diagnosis-and-treatment-on-medication-adherence-in-youth-with-systemic-lupus-erythematosus/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-psychiatric-diagnosis-and-treatment-on-medication-adherence-in-youth-with-systemic-lupus-erythematosus/