Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose : In cross-sectional studies, depression and pain in other locations have been reported as predicting poorer outcomes following total knee and hip arthroplasty. These factors may be better explained by a common pathophysiology of aberrant central pain processing as is seen in conditions like fibromyalgia. We hypothesized that patients with altered central pain processing would be less likely to report pain improvement after lower extremity joint arthroplasty.
Methods : Patients were preoperatively phenotyped using validated self-reported, including the Brief Pain Inventory, PainDETECT, WOMAC, Hospital Anxiety and Depression Scale, Catastrophizing, health information (opioid use, ASA Status, BMI, primary anesthetic), and demographics. Participants also completed the American College of Rheumatology (ACR) survey criteria for fibromyalgia as a surrogate of centralized pain, which is a measure of widespread pain and an assessment of symptoms such as fatigue or trouble thinking. Patients were re-assessed using the same preoperative phenotype at 6-months postoperatively. Data were analyzed using R 2.15.2. A linear model was used to regress the change in pain responses at surgical site and overall on a set of covariates including the baseline pain value.
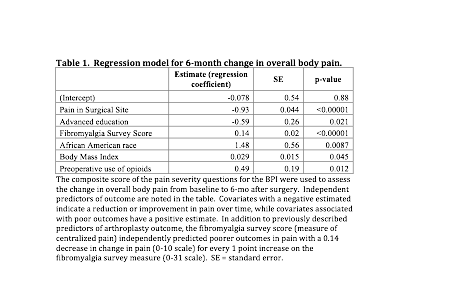
Results : 598 of the 851 patients approached agreed to participate (70.3%). A total of 454 patients completed the 6-month outcome follow-up (75.9%) and were included in the outcome analyses. Preoperatively, patients with higher fibromyalgia survey scores were significantly younger, more likely to be female, less educated, more likely to be on disability or unemployed, and more likely to be taking preoperative opioids (p < 0.05 for each comparison). Patients with higher scores on the fibromyalgia survey also reported higher pain severity overall and at the surgical site, higher WOMAC scores, and had a more negative psychological profile (p < 0.0001 for each comparison). When adjusting for other covariates, patients with higher preoperative pain and educational status showed more improvement in overall pain (Table 1). Higher fibromyalgia survey scores, higher BMI, use of opioids preoperatively, and African American race were independently predictive of less improvement in pain overall. Similar results were obtained when regressing for the change in surgical site pain.
Conclusion : In this large, prospective, observational cohort study, the ACR survey criteria for fibromyalgia differentiated patients preoperatively and was independently predictive of poorer long-term outcomes when assessing both the change in the surgical site and overall body pain. Altered central pain processing may explain some of the variance in outcomes previously described in lower extremity joint arthroplasty. This simple, validated, self-report measure may add value in selecting appropriate candidates for arthroplasty.
Disclosure:
C. M. Brummett,
Purdue Pharma L.P.,
5;
A. Urquhart,
None;
B. Hallstrom,
None;
A. Tsodikov,
None;
D. A. Williams,
Purdue Pharma L.P.,
5,
Forest Pharmaceuticals,
5,
Pfizer Inc,
5;
D. J. Clauw,
Nuvo, Merck, Cerephex, Pfizer,
2,
Lilly, Pfizer, Forest, Nuvo, Cerephex, Purdue,
5.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-centralized-pain-on-long-term-analgesic-response-to-lower-extremity-joint-arthroplasty-a-prospective-observational-cohort-study/