Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose:
SLE is a chronic illness that carries both a physical and psychosocial burden, where the cumulative impact can lead to worse global outcomes. One outcome of interest is BMI especially with recent public health efforts highlighting the risk of BMI elevation to obesity and its affiliated metabolic risk factors. We examined the associated features and impact of BMI variability amongst SLE patients.
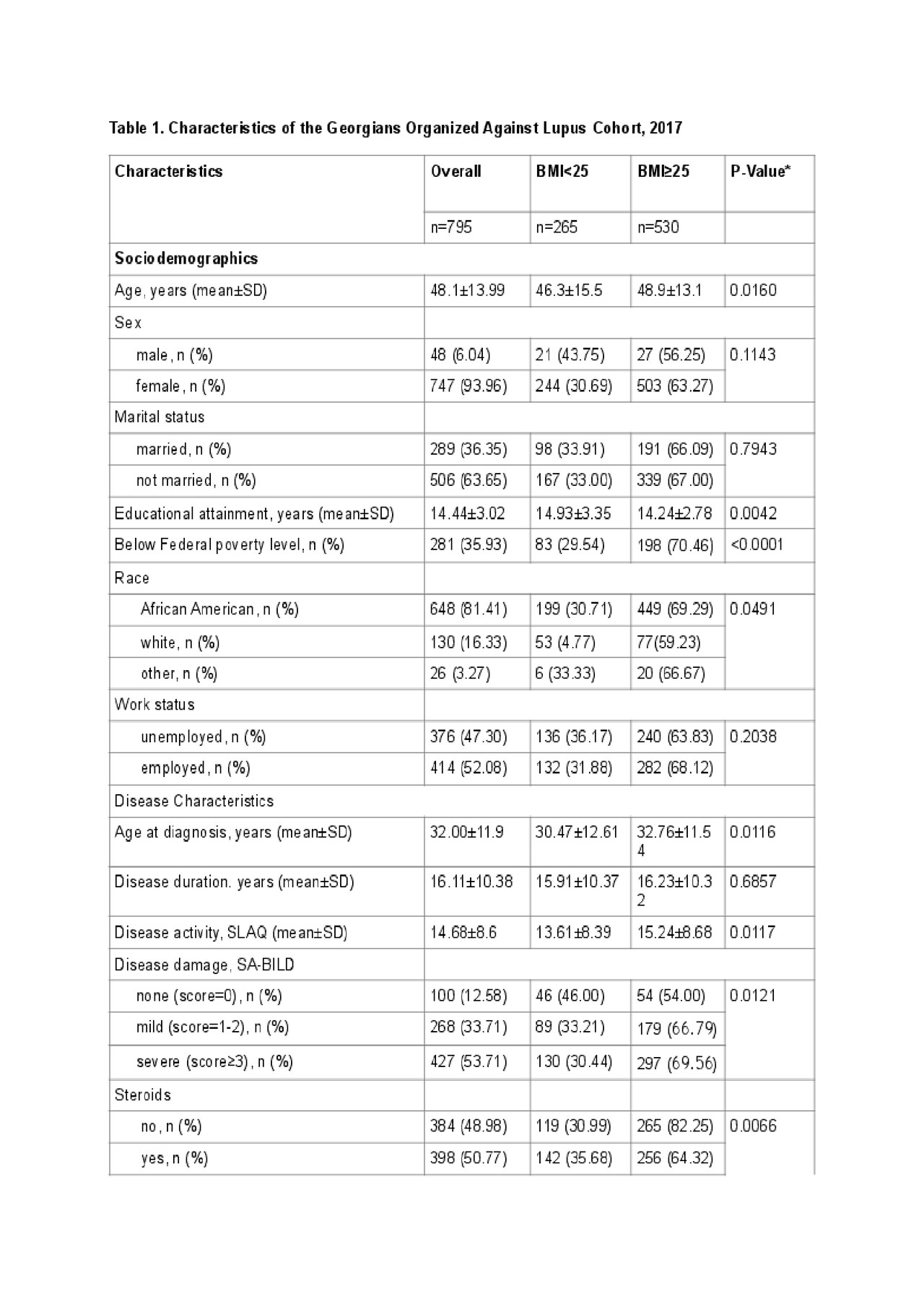
Methods: The Georgians Organized Against Lupus (GOAL) is a population-based research cohort of SLE patients in Atlanta derived from the Centers for Disease Control and Prevention supported by Georgia Lupus Registry who consent to and complete annual surveys encompassing multiple domains. The 2017 results included calculated BMI and the Patient-Reported Outcomes Measurement Information System (PROMIS) questionnaire for depression with T-score conversion, disease activity (Systemic Lupus Activity Questionnaire, SLAQ), perceived stress (Perceived Stress Scale), discrimination (Everyday Discrimination Scale), and self-assessment of continuity of care with a regular provider. Logistic regression evaluated the potential relationship between BMI and aforementioned factors. BMI was categorized as either non-elevated (BMI< 25) or elevated (BMI≥25).
Results: The 2017 GOAL survey comprised of 795 patients, of whom 265 (33.3%) had non-elevated BMI and 530 (66.6%) had elevated BMI. African Americans (AA) made up 81.4% of this cohort. The average disease duration was 16.11 ± 10.38 years. Univariate logistic regression analyses demonstrated that older age was linked to elevated BMI (p = 0.016, Table 1). Additionally, greater years of higher education was linked to non-elevated BMI, p=0.0042; whereas being below the federal poverty level and/or being AA carried greater association with elevated BMI (p< 0.001 and p=0.0491, respectively). While disease duration carried no impact on BMI, diagnosis at a later age was linked to higher incidence of elevated BMI, p=0.0116. Patients with elevated BMI had greater disease activity and damage and experienced more discrimination.
Conclusion:
The variability of BMI amongst SLE can be associated with different clinical and behavioral impact. Patients with greater disease activity had elevated BMI. They were also likelier to experience more discrimination, but this may be affected by the greater proportion of AA’s (81.4%) in the cohort. Poverty was associated with elevated BMI. Further research into understanding the prolonged impact of BMI variability in SLE needs to be investigated and can prove to be instrumental in the overall care of SLE patients.
To cite this abstract in AMA style:
Gao X, Vashi T, Lim S. The Impact of Body Mass Index Variability in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-body-mass-index-variability-in-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-body-mass-index-variability-in-systemic-lupus-erythematosus/