Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular morbidity and mortality is a well-established problem in patients with systemic lupus erythematosus (SLE). Hydroxychloroquine (HCQ) has been seen as a potential atheroprotective agent.The aim of this systematic review was to assess the impact of HQC on traditional and nontraditional cardiovascular markers in patients with SLE.
Methods: A search of MEDLINE, Embase and the Cochrane library for randomized controlled trials (RCTs) or cohort studies evaluating the impact of antimalarials on cardiovascular (CV) markers in patients with SLE was conducted up to January 2020. Data extraction included traditional (lipid profile, diabetes, blood pressure [BP]) and nontraditional CV markers (glycosylated hemoglobin levels, insulin resistance, high sensitivity C-reactive protein, homocystein concentrations, IgG anti-apolipoprotein A1 [anti-apoA1], endothelial function, arterial stiffness, arterial elasticity and coronary artery calcification [CAC]). The methodological quality was assessed using the QUIPS risk of bias tool for observational studies and the Cochrane Risk of Bias Assessment Tool for RCTs. A narrative synthesis of the findings was presented, and a meta-analysis will be conducted if appropriate. The review was registered on PROSPERO (CRD42020162067).
Results: The search strategy produced 715 articles, of which 24 and 14 were extracted (16,717 SLE patients) for quantitative and qualitative analysis, respectively. Only one RCT and 37 observational studies were included. The follow-up period varied widely in longitudinal studies, ranging from 3 months to 9.3 years. Table 1 shows a summary of findings with mean differences or effect size from pooled studies. The mean differences in VLDL-cholesterol, triglycerides, and diastolic BP were significantly lower in patients on antimalarial therapy compared to those without antimalarial therapy, and HLD-cholesterol was significantly higher in the former group. Within-group analysis showed significantly lower total cholesterol and LDL-cholesterol after antimalarial therapy. Moreover, patients on antimalarials had a lower risk of prevalence and incidence of diabetes than patients not on antimalarials. HCQ use was protective and was associated with lower BP variability. However, the risk of prevalent hypertension or IgG anti-apoA1 was not significantly lower in patients with antimalarial therapy. The benefit of antimalarial therapy on endothelial function and arterial stiffness was unclear. The QUIPS tool showed a low-to-high RoB, and GRADE showed very low to low quality of evidence per outcome.
Conclusion: There is some evidence from observational studies on associations between antimalarial therapy and some CV outcomes. However, the data on which this conclusion was based was of very low to low evidence. This emphasizes the need for higher quality studies to resolve uncertainties.
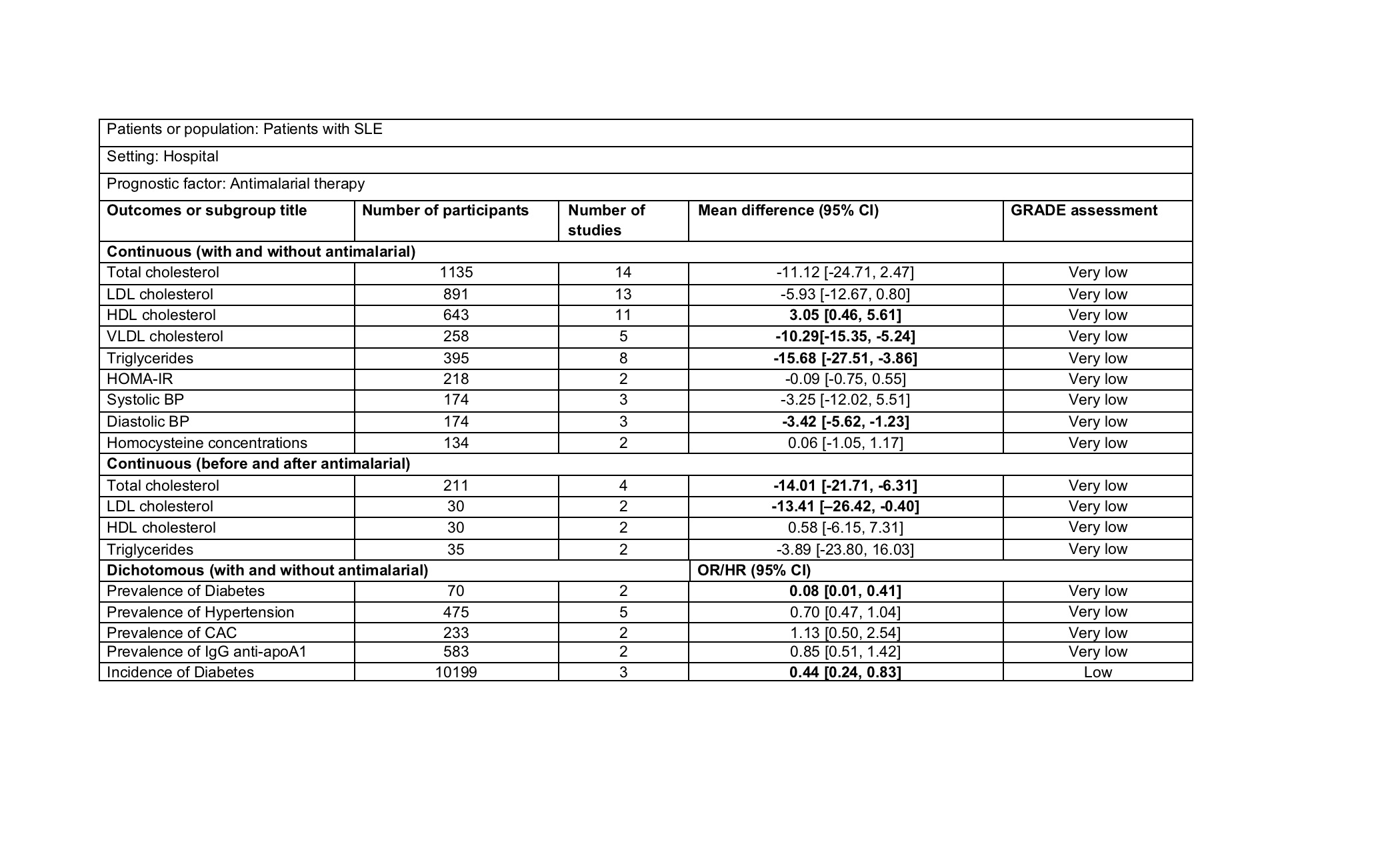 Table 1. Modified GRADE summary of findings on the influence of antimalarial therapy on cardiovascular outcomes
Table 1. Modified GRADE summary of findings on the influence of antimalarial therapy on cardiovascular outcomes
To cite this abstract in AMA style:
Mendoza-Pinto C, Garcia-Carrasco M, Munguía-Realpozo P, Etchegaray-Morales I, Mendez-Martínez S. The Impact of Antimalarial Agents on Traditional and Non-traditional Cardiovascular Markers in Patients with Systemic Lupus Erythematosus: A Systematic Review and Meta-analysis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-antimalarial-agents-on-traditional-and-non-traditional-cardiovascular-markers-in-patients-with-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-antimalarial-agents-on-traditional-and-non-traditional-cardiovascular-markers-in-patients-with-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/
