Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The American College of Rheumatology defines amplified musculoskeletal pain syndrome (AMPS) as the umbrella term for non-inflammatory musculoskeletal pain, and most commonly occurs in childhood and adolescence. AMPS is often seen in children with preceding diagnosis of rheumatic disease; however, it is often difficult to identify AMPS among pediatric patients suffering from painful inflammatory disease. This study aimed to 1) describe children with dual diagnoses of amplified pain and rheumatologic disease with the goal of finding which rheumatologic diseases are most represented among those with both conditions and 2) describe factors associated with subspeciality amplified pain clinic referral.
Methods: We conducted a retrospective chart review of all patients ≤18 years who presented to the pediatric rheumatology clinic at The Children’s Hospital of Philadelphia between 1/1/2012 and 12/31/2019. Participants were selected who had a diagnosis code for amplified musculoskeletal pain syndrome. Demographic data, concomitant medical diagnoses, and rheumatic diagnoses were abstracted, as well as time to AMPS diagnosis and referral to AMPS clinic. Descriptive statistics were reported in terms of medians and interquartile ranges (IQR) for continuous variables and as absolute frequencies and percentages for categorical variables. We compared the characteristics between those referred and not referred to AMPS clinic using Pearson’s chi squared and Wilcoxon-rank sum, as appropriate. All p≤0.05 were considered statistically significant.
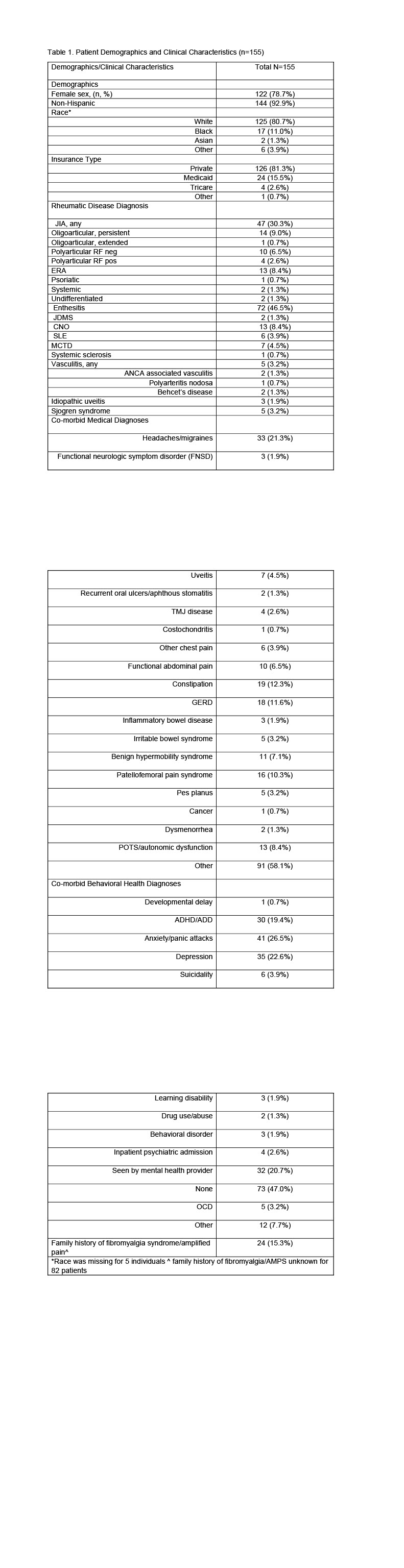
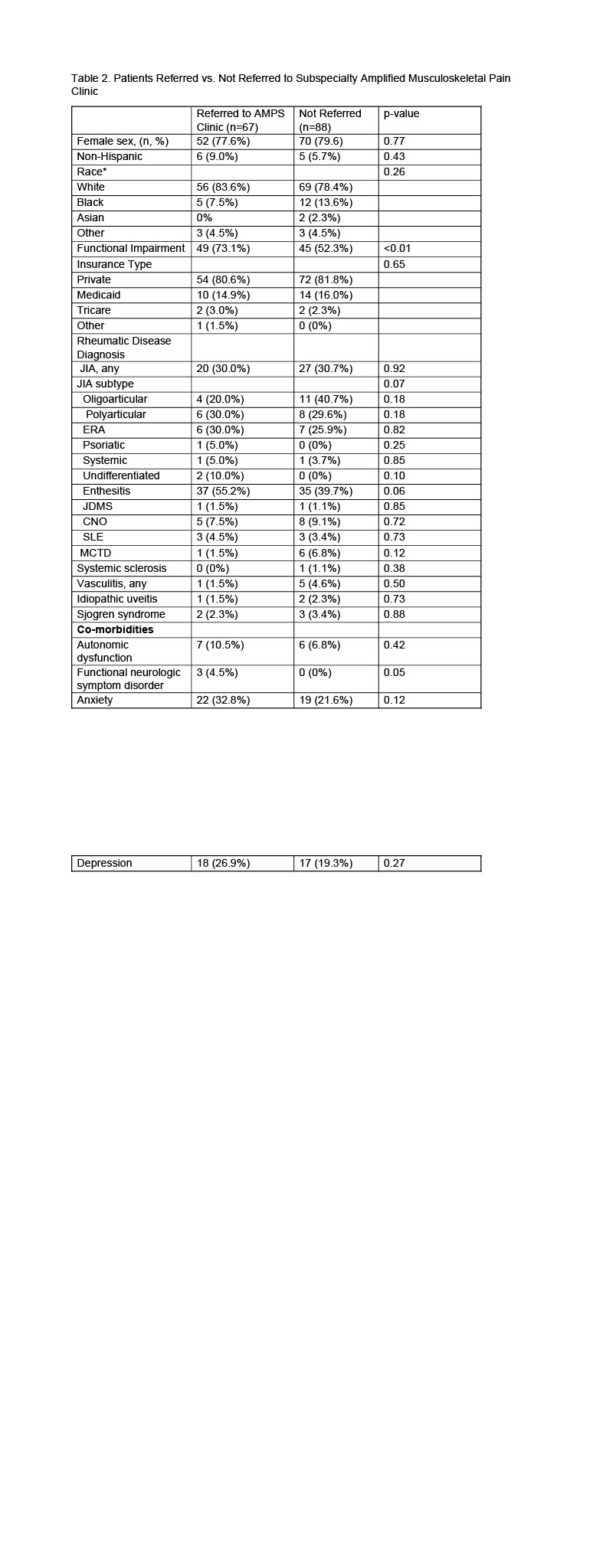
Results: We identified 155 patients with both amplified pain and rheumatic disease. Most patients had rheumatic disease only (72.9%) at their initial rheumatology visit, and about 1/5 (18.7%) had a dual diagnosis. Only 8% (n=13) presented with AMPS first. For those who were diagnosed with a rheumatic disease first, time to AMPS diagnosis (secondary amplified pain) was a median of 9 (IQR: 1.3, 27.7) months. The majority were white (80.7%), non-Hispanic (92.9%), female (78.7%) and had private insurance (81.3%) (Table 1). The most common rheumatic diseases were enthesitis (46.5%), JIA (30.3%), and CNO (8.4%). A little less than half (43.5%; n=67) were referred to the dedicated amplified pain clinic and 85.1% (n=57) of those referred completed a new patient visit in the AMPS clinic. Those with significant functional impairment and those with functional neurological symptom disorder were the only factors associated with AMPS clinic referral (Table 2).
Conclusion: Of children with co-morbid AMPS and rheumatic disease seen in a rheumatology clinic at a tertiary care center, rheumatic disease most often presents first. The most represented diseases were JIA, enthesitis and CNO and average time to AMPS diagnosis was about 1-2 years. Our findings suggest that pediatric rheumatologists at our center are comfortable managing amplified pain, reserving referrals only for those with significant functional impairment. Based on these findings, prevention programs for secondary amplified pain may best be targeted towards children with JIA, enthesitis and CNO and soon after diagnosis.
To cite this abstract in AMA style:
Ruthen S, McGill M, Butler N, Abel D, Argraves M, Gmuca S. The Exploration of Secondary Amplified Musculoskeletal Pain Syndrome (AMPS) in Pediatric Patients with Rheumatologic Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-exploration-of-secondary-amplified-musculoskeletal-pain-syndrome-amps-in-pediatric-patients-with-rheumatologic-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-exploration-of-secondary-amplified-musculoskeletal-pain-syndrome-amps-in-pediatric-patients-with-rheumatologic-disease/