Session Information
Date: Sunday, November 13, 2016
Title: Rheumatoid Arthritis – Small Molecules, Biologics and Gene Therapy I: Treatment Strategies
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Should we aim at remission if patients are in low disease activity (LDA)? We assessed if rheumatoid or undifferentiated arthritis (RA, UA) patients who achieved LDA benefit with better functional ability from treatment intensification aimed at DAS remission.
Methods: In the IMPROVED study 610 patients with early RA (ACR 2010) or UA were ‘treated to target’ aimed at DAS remission, assessed every 4 months. Initial treatment was methotrexate (MTX) + tapered high dose prednisone. Patients with DAS≤1.6 tapered treatment. Patients with DAS>1.6 were randomized to MTX + hydroxychloroquine + sulphasalazine + prednisone or to MTX + adalimumab. Over 5 years, patients with DAS>1.6 were required to increase, change or restart medication. HAQ was measured 4-monthly. A linear mixed model analysis with random intercept and independent covariance matrix was performed to test the relationship between changes in therapy and HAQ over time. Patients in LDA with DAS>1.6 with and without (i.e. protocol violation) treatment change were compared. ΔHAQ and ΔDAS at each visit compared to the previous visit were calculated. We tested the interaction effect between change in treatment and follow-up time adjusted for possible confounders.
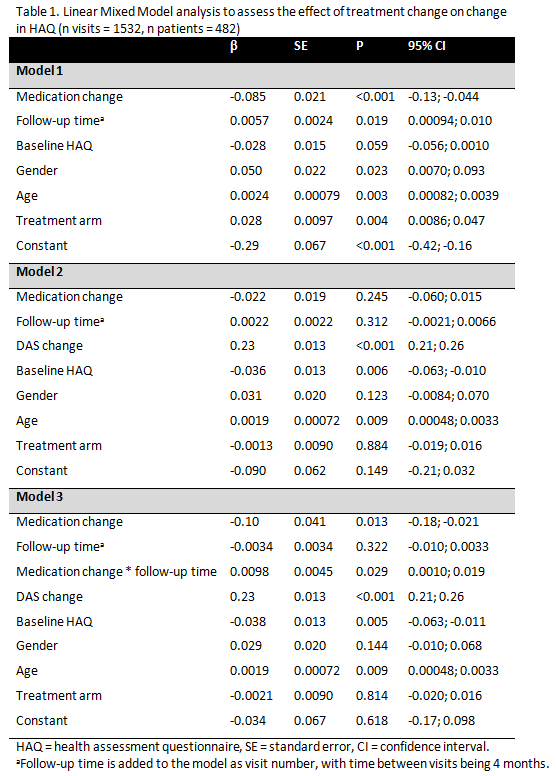
Results: Over 5 years DAS and HAQ showed a statistically significant and clinically relevant decrease [Baseline HAQ mean (SD) 1.2 (0.7), ΔHAQ -0.59, 95% CI -0.61, -0.57; Baseline DAS mean (SD) 3.2 (1.7), ΔDAS -1.77, 95% CI -1.79; -1.75]. The number of patients in LDA per visit ranged from 88 to 146, of which 26% to 73% had no treatment change, with an increase in such protocol violations towards the end of study. We found a statistically significant but not clinically relevant effect of treatment change on ΔHAQ, corrected for baseline HAQ, age, gender and treatment arm (model 1, β -0.085, 95% CI -0.13, -0.044). When ΔDAS was added (model 2), treatment change was partly explained by ΔDAS and the effect of treatment change was no longer statistically significant (β -0.022, 95% CI -0.060; 0.015). When the interaction between treatment change and time in follow-up was added (model 3), a statistically significant interaction was found (β 0.0098, 95% CI 0.0010; 0.019), indicating a lower improvement in HAQ after treatment change if follow-up time increased (table 1).
Conclusion: During 5 years of DAS remission steered treatment in early RA or UA patients, treatment intensification or change for patients already in LDA resulted in a statistically significant but not clinically relevant improvement in HAQ, which was partly explained by ΔDAS. The effect decreased with increasing follow-up time. This supports the call for rapid treatment start to suppress disease activity in order to restore physical functioning. Remission may be the optimal goal, but when patients are in longer follow-up and HAQ is acceptably low, it might be sufficient to accept LDA rather than continue treatment changes aiming at remission.
To cite this abstract in AMA style:
Bergstra S, Olivas Vergara O, Akdemir G, Steup-Beekman G, Ronday H, Harbers J, Landewé R, Allaart C. The Effect of Treatment Adjustments Aimed at DAS Remission on Physical Functioning in Undifferentiated and Rheumatoid Arthritis Patients in Low Disease Activity [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/the-effect-of-treatment-adjustments-aimed-at-das-remission-on-physical-functioning-in-undifferentiated-and-rheumatoid-arthritis-patients-in-low-disease-activity/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-effect-of-treatment-adjustments-aimed-at-das-remission-on-physical-functioning-in-undifferentiated-and-rheumatoid-arthritis-patients-in-low-disease-activity/