Session Information
Date: Monday, November 14, 2022
Title: Abstracts: Cognition and Behavior in RA and Systemic Sclerosis
Session Type: Abstract Session
Session Time: 3:00PM-4:00PM
Background/Purpose: Insomnia is highly prevalent in people with rheumatoid arthritis (RA) and may exacerbate symptoms and burdens, such as fatigue, depressive symptoms, and pain (1). Cognitive behavioral therapy for insomnia (CBT-I) has been shown to produce positive effects on sleep in other clinical populations (2,3). However, CBT-I has not previously been investigated in people with RA (1).
The primary objective was to compare the effect of nurse-led group-based CBT-I to usual care on sleep efficiency, measured by polysomnography (PSG) immediately after the intervention (i.e. seven weeks after baseline) in people with RA. Secondary objectives included comparing the longer-term effect of CBT-I on sleep and RA-related outcomes at 26 weeks’ follow-up.
Methods: In a randomized controlled trial (ClinicalTrials.gov Identifier NCT03766100), using a parallel-group design, the experimental intervention was six weeks of CBT-I; the control comparator was usual care. CBT-I was delivered face-to-face by a CBT-I trained nurse. The primary analyses were based on the intention-to-treat (ITT) population; missing data were statistically handled using repeated-measures linear mixed-effects models adjusted for the level at baseline.
Results: The ITT population consisted of 62 participants (89% women), with an average age of 58 years (SD 10), DAS28-CRP of 3.4 (SD 1.0), Insomnia Severity Index (ISI) score of 18.9 (SD 4.4) and median Patient Global Assessment score of 55 (IQR 28;71).
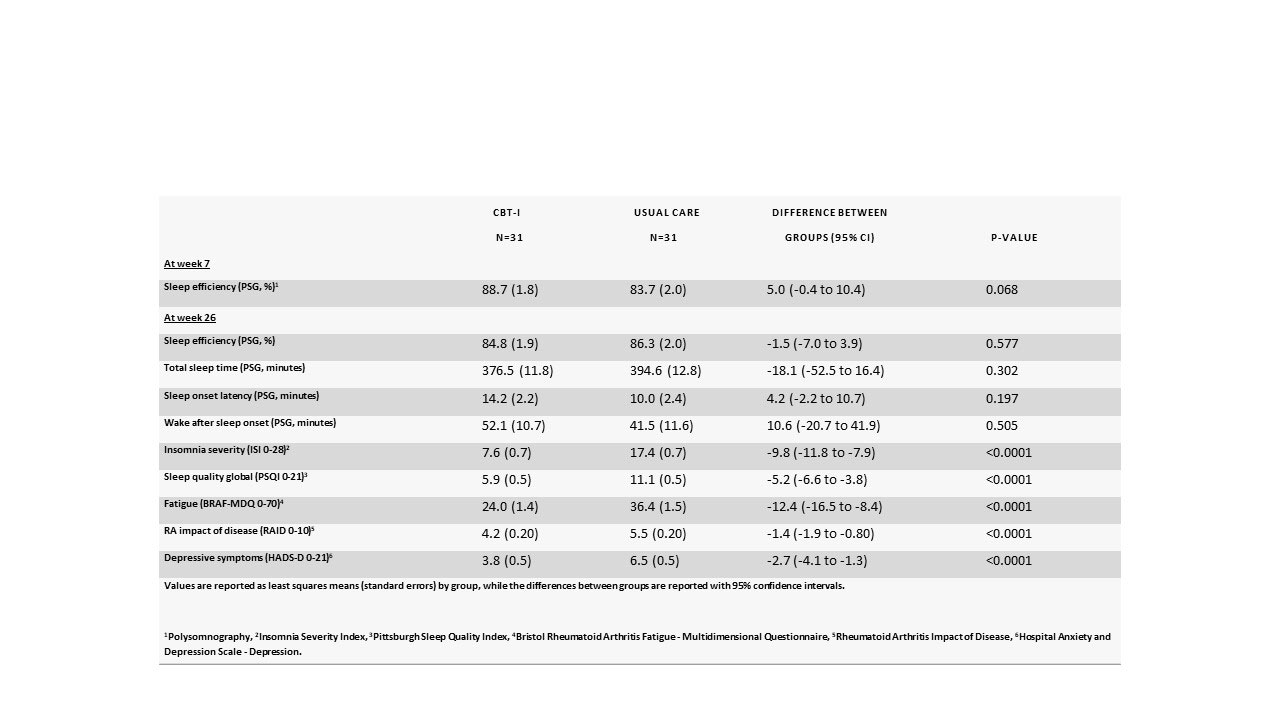
When the primary outcome was measured by PSG at week seven, sleep efficiency was 88.7% in the CBT-I group, compared to 83.7% in the control group (difference: 5.0 [95% CI -0.4 to 10.4]; p=0.068) (See Table 1). Secondary outcomes measured by PSG had not improved at week 26 either.
However, for all secondary sleep and RA-related patient-reported outcomes, there were statistically highly significant differences between CBT-I and usual care e.g. Insomnia Severity Index (ISI, range 0-28, higher is worse): -9.8 [95% CI -11.8 to -7.9], RA impact of disease (RAID, range 0-10, higher is worse) -1.4 [95% CI-1.9 to -0.80] and Patient Global Assessment (range 0-100, higher is worse): -13.0 [95% CI -20.9 to -5.1] at 26 weeks’ follow-up.
Conclusion: Nurse-led, group-based CBT-I for two hours per week for six weeks, did not improve objectively measured sleep efficiency or any other outcomes measured by PSG. However, CBT-I showed long-term improvement on patient-reported outcomes such as fatigue, impact of disease, depression, pain, and Patient Global Assessment – a finding that could have important clinical implications.
References
(1) PMID: 25620673
(2) PMID: 16804151
(3) PMID: 26434673
To cite this abstract in AMA style:
Latocha K, Loeppenthin K, Østergaard M, jennum p, Hetland M, Rogind H, Lundbak T, Midtgaard J, Christensen R, Esbensen B. The Effect of Group-based Cognitive Behavioral Therapy for Insomnia in People with Rheumatoid Arthritis: A Randomized Controlled Trial [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-effect-of-group-based-cognitive-behavioral-therapy-for-insomnia-in-people-with-rheumatoid-arthritis-a-randomized-controlled-trial/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-effect-of-group-based-cognitive-behavioral-therapy-for-insomnia-in-people-with-rheumatoid-arthritis-a-randomized-controlled-trial/