Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammatory back pain (IBP) as a symptom has been shown to perform effectively for selecting patients in primary care / orthopaedic settings for referral of chronic back pain patients to the rheumatologist for further diagnostic work-up. IBP is also being used as a diagnostic test of axial spondyloarthritis (axSpA) by rheumatologists, but no validations studies have been performed so far with IBP as a diagnostic tool. The aim of the DIVERS study was to evaluate the diagnostic value of the IBP symptom in axSpA in the rheumatology setting.
Methods:
A total of 405 consecutive patients referred to a rheumatologist because of chronic back pain starting at an age <45 years and suspicion of axSpA were included in this multicentre study. A questionnaire containing all relevant IBP parameters was first answered by the patient, followed by a rheumatologist blinded for presence or absence of other SpA features and for the diagnosis, and finally by the rheumatologist responsible for the diagnosis. A global evaluation of IBP by rheumatologists, and IBP according to the previously published Calin’s, Berlin and ASAS criteria as well as single items of IBP were compared regarding their diagnostic performance.Results:
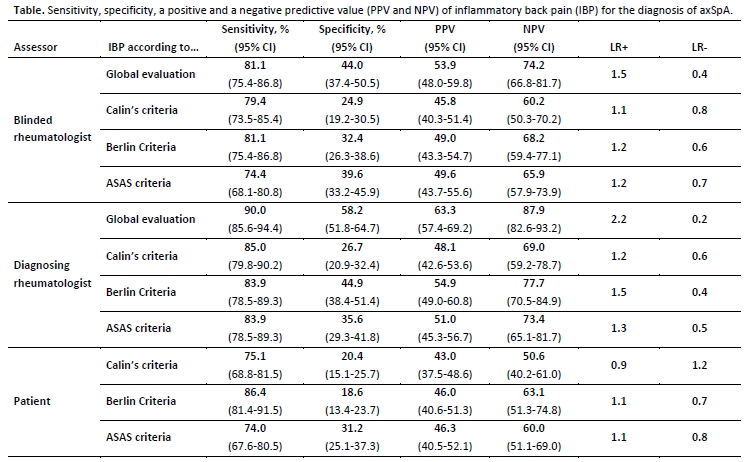
The diagnosis of definite axSpA was made in 180 (44.4%) patients (88 with ankylosing spondylitis and 92 with non-radiographic axSpA). The sensitivity, specificity and the positive likelihood ratio of IPB for the axSpA diagnosis was 81%, 44%, and 1.5, respectively, if globally assessed by the blinded rheumatologist, and 90%, 58% and 2.2, respectively, if globally assessed by the diagnosing rheumatologist – table. There was no clear superiority of any of the three criteria sets regarding sensitivity for the axSpA diagnosis with an overall sensitivity of about 80% and specificity between 25% and 45% if symptoms were assessed by a rheumatologist – table. The performance of the criteria sets based on patient’s own evaluation of IBP symptoms was generally lower. No single IBP parameter showed superiority regarding sensitivity or specificity in comparison to the criteria sets.Conclusion:
IBP demonstrated high sensitivity but rather modest specificity for the diagnosis of axSpA among patients with chronic back pain referred to a rheumatologist. A resulting moderate diagnostic value of IBP in the rheumatology setting is likely to be counterbalanced by increase in the pre-test probability of axSpA in this patients population.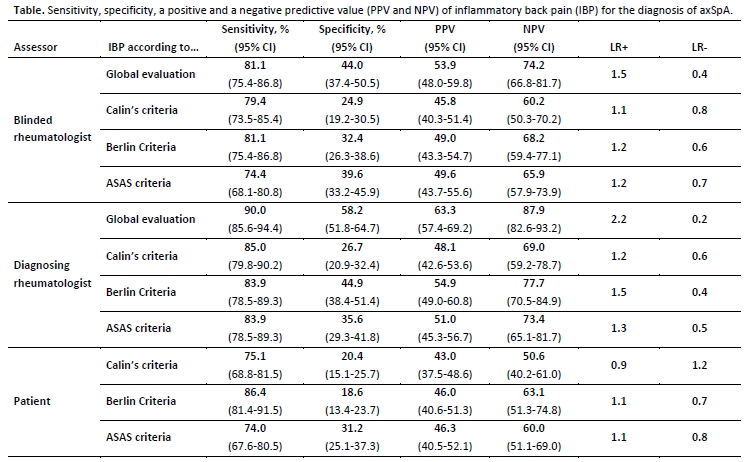
Disclosure: D. Poddubnyy, None; I. Spiller, None; J. Listing, None; J. Braun, None; J. Sieper, None; M. Rudwaleit, None.
To cite this abstract in AMA style:
Poddubnyy D, Spiller I, Listing J, Braun J, Sieper J, Rudwaleit M. The Diagnostic Value of the Symptom of Inflammatory Back Pain in the Rheumatology Setting [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/the-diagnostic-value-of-the-symptom-of-inflammatory-back-pain-in-the-rheumatology-setting/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-diagnostic-value-of-the-symptom-of-inflammatory-back-pain-in-the-rheumatology-setting/
