Session Information
Date: Tuesday, November 7, 2017
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's – Clinical Aspects and Therapeutics Poster III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc, scleroderma) patients can have the end-stage vasculopathy manifestation of a digital ulcer (DU). Brachial artery flow mediated dilation (FMD) is an established non-invasive vascular marker of endothelial function in SSc. We hypothesized that FMD could stratify the timeline of DU development and role of vasodilators in management.
Methods: Patients were recruited from our scleroderma center at the time of a routine care visit. All vascular measures were assessed by duplex ultrasound Doppler at baseline and after 6 months follow-up for up to two years. Specifically, resting brachial artery blood flow, shear rate, and diameter and BP cuff induced ischemia, vascular reactivity (peak reactive hyperemia), vascular shear rate (peak hyperemia/area under the curve [AUC]), and FMD (Δmm and %) were measured for 2 min after cuff release. We examined FMD variables in SSc patients that (1) had a DU at baseline, (2) developed a new DU, and (3) never had DU in up to 24 months of follow-up. General linear models were used to compare these continuous variables between SSc patients with and without DU controlling for the days from baseline FMD measurement and use of any vasodilatory drug.
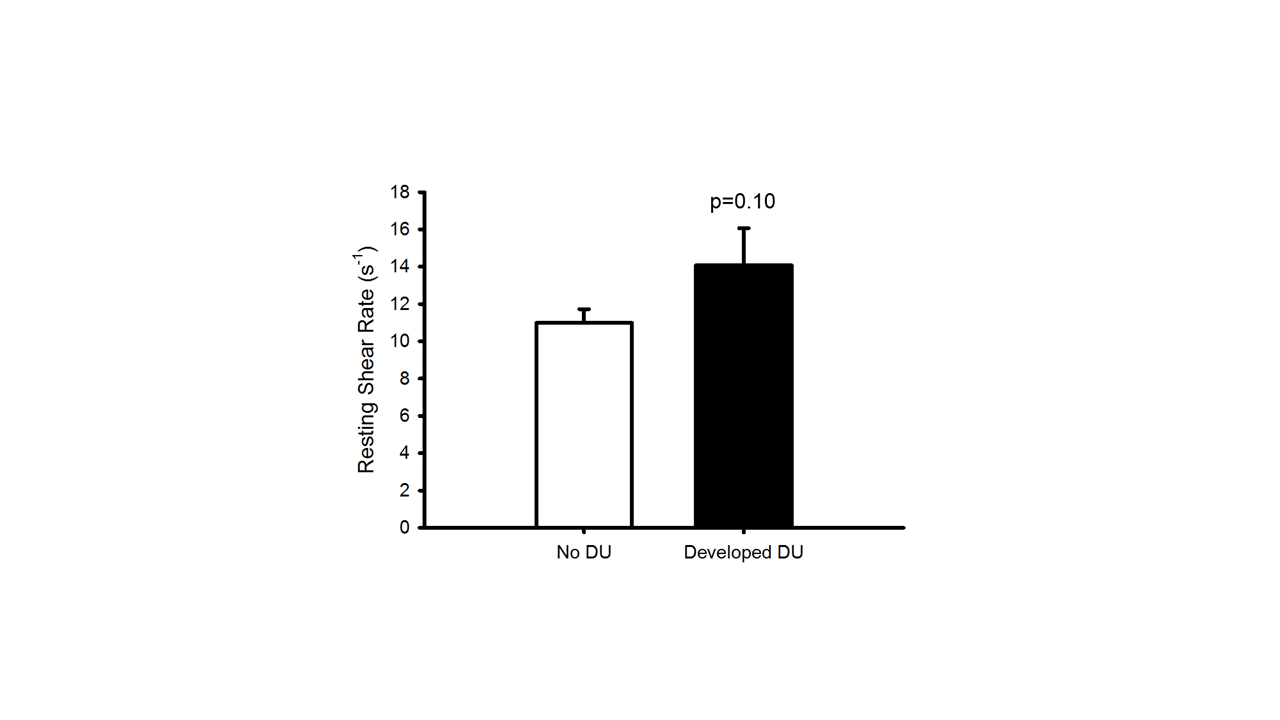
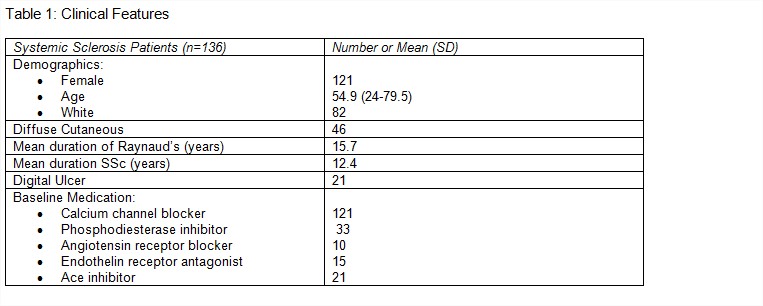
Results: FMD was determined in 136 SSc patients at baseline and 55 patients in follow-up. Baseline SSc clinical features are described in Table 1. In those patients with follow-up FMD, 10 (48%) with a baseline DU healed over the course of two years. The timeline for healing for initial DU patients included 3 within 12 month and 4 within 18 months. Seven of 115 patients with no DU at baseline developed a DU at the time of repeat FMD measures. Resting blood flow differed between patients with healed DU and developed DU, in that they had higher blood flow at baseline (p=0.03), which correlated to vasodilator use. When FMD variables were analyzed over time, resting arterial wall shear rate increased over time for all patients and was lowest for those with no DU. The difference in the DU groups (developed and no DU) trended towards significance (p=0.10, Figure 1).
Conclusion: FMD applied to routine clinical care of SSc patients identified that DU trial length may require up to 18 months to document complete healing. FMD variables may be important secondary outcome measures in DU trials. Higher resting blood flow in individuals with a healed DU and those who never had a DU supports the role of vasodilators for this indication. The role of therapeutics that reduce vascular shear rate may be an opportunity for both SSc-DU prevention and healing.
Figure 1: Follow-up vascular shear rate of SSc patients (mean, SEM) that never had DU (n=41) versus developed DU (n=7).
To cite this abstract in AMA style:
Frech TM, Machin D, Murtaugh M, Donato A. The Clinical Utility of Flow-Mediated Dilation in Systemic Sclerosis Digital Ulcer Assessment [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/the-clinical-utility-of-flow-mediated-dilation-in-systemic-sclerosis-digital-ulcer-assessment/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-clinical-utility-of-flow-mediated-dilation-in-systemic-sclerosis-digital-ulcer-assessment/