Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The clinical relevance of different antiphospholipid antibody (aPL) profiles, including low level anticardiolipin (aCL) and anti β2-glycoprotein-I (aβ2GPI) antibodies, is ill-defined in the pediatric population. The purpose of this project is to describe the demographic, clinical, and laboratory characteristics of aPL “positive” pediatric patients based on different aPL profiles.
Methods: In this single center retrospective cohort study, based on the screening of our pediatric (age ≤18yo) rheumatology electronic medical records (2016—2022), we identified patients who had at least one “positive” aPL (lupus anticoagulant [LA], aCL IgG/M, or aβ2GPI IgG/M) result. First, we grouped patients based on initial high- (LA positive and/or aCL/aβ2GPI IgG/M≥40U [ELISA]) vs low- (LA negative and aCL/aβ2GPI IgG/M 20-39U) risk aPL profiles to evaluate subsequent aPL testing frequency and results. Secondly, we descriptively analyzed the demographic and clinical characteristics of patients with persistently positive (at least 12 weeks apart) aPL results based on different aPL profiles.
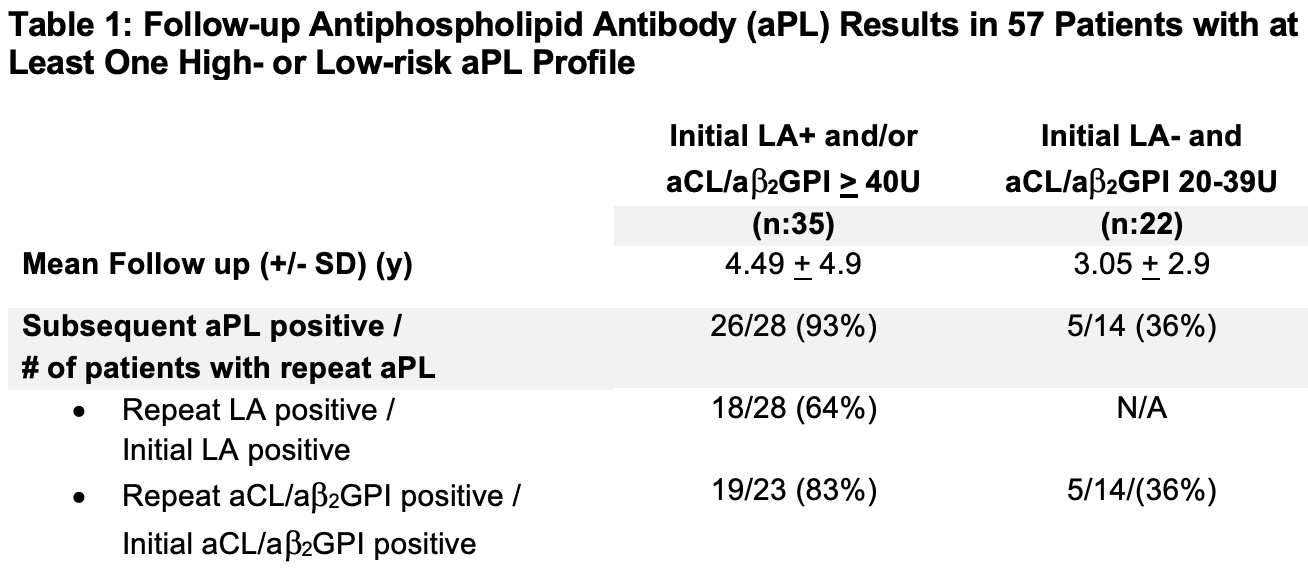
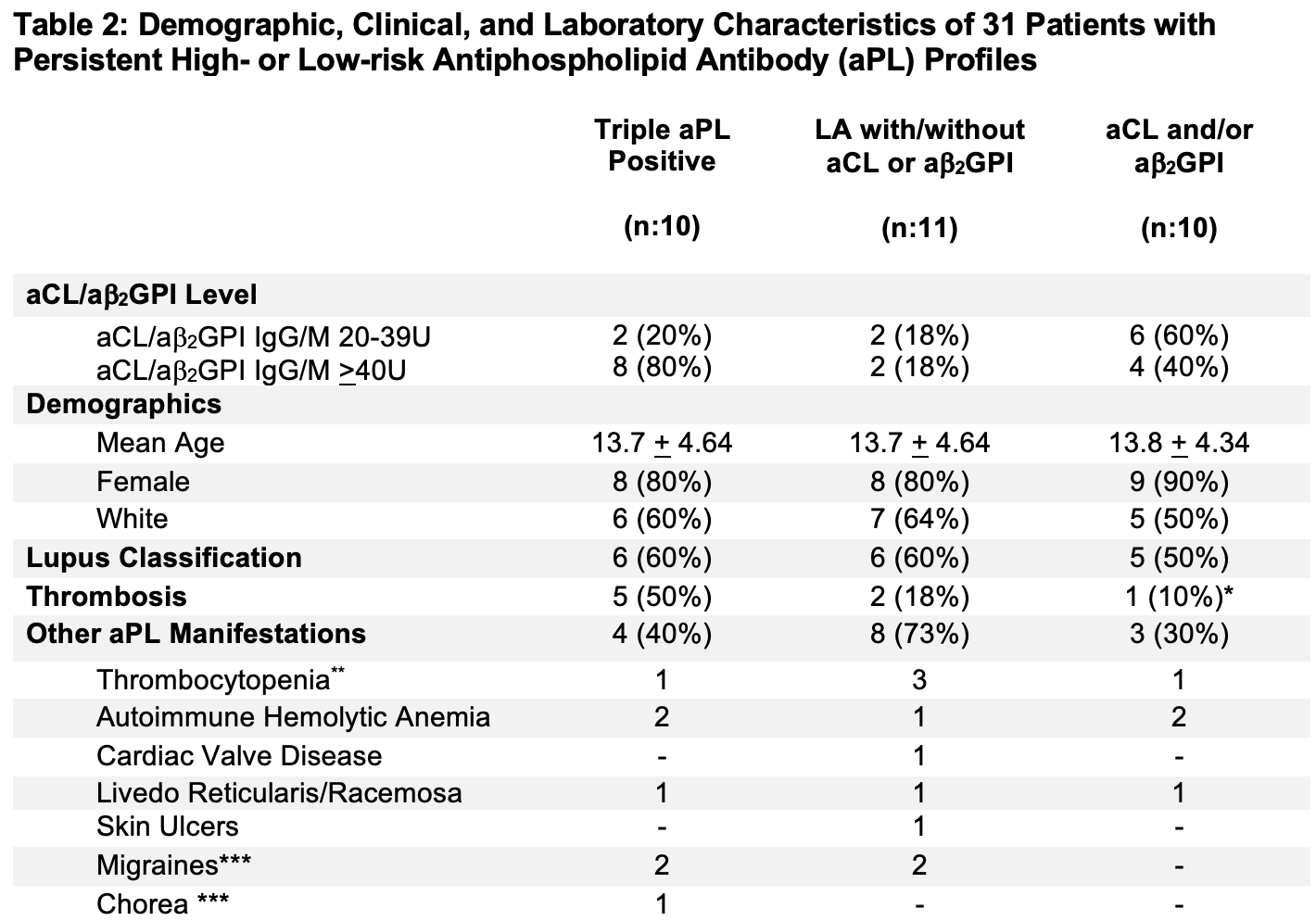
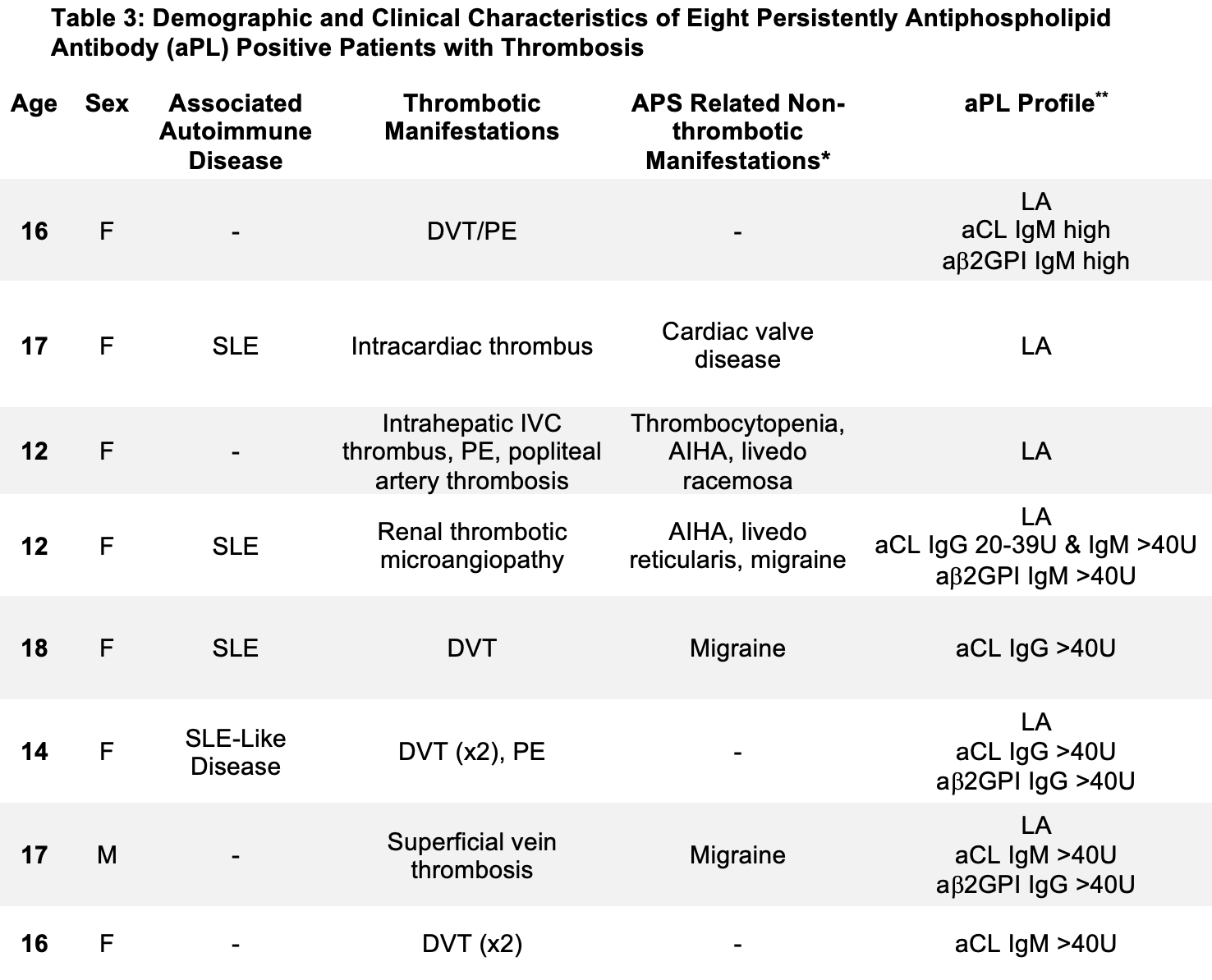
Results: Of 113 aPL “positive” patients identified, 56 (50%) were excluded as they had very low aCL/aβ2GPI IgG/M positivity (above laboratory normal range but < 20U). Of the remaining 57 patients (female: 48 [84%], lupus classification: 21 [37%]), 35 (61%) had an initial high-risk profile and 22 (39%) had an initial low-risk profile. Based on the subsequent aPL results available in 42/57 (74%) patients, 26/28 (93%) in the high-risk, and 5/14 (36%) in the low-risk group remained still positive (Table 1). Of these 31 patients with persistent aPL positivity, thrombosis occurred in eight (26%) patients with high-risk aPL profile and in none with low-risk aPL profile; other aPL-related manifestations were reported in 15 (48%) patients with persistent aPL positivity (Tables 2 and 3). Of 26 patients without persistent aPL results (repeat test either negative or not available), none developed thrombosis, one had livedo reticularis, and two had migraines.
Conclusion: An initial low-risk aPL profile (negative LA and aCL/aβ2GPI IgG/M levels 20-39U) is persistent in only approximately one-third of the pediatric patients, which was not associated with thrombosis in our cohort. Meanwhile, a high-risk profile defined as LA positivity and/or aCL/aβ2GPI IgG/M levels ≥ 40U is persistent in 90% of pediatric patients, about a third of whom had history of thrombosis, and half had non-thrombotic aPL-related manifestations. Our results underscore the need for a large-scale international effort to better characterize the aPL-related manifestations in pediatric patients with persistent high-risk aPL-profiles, which can eventually guide the development of future pediatric-specific APS classification criteria.
F: Female; DVT: Deep venous thrombosis; PE: Pulmonary embolism; IVC = inferior vena cava; SLE: systemic lupus erythematosus; AIHA: autoimmune hemolytic anemia. LA: lupus anticoagulant; aCL: anticardiolipin antibody; and aB2GPI: anti-beta_2 glycoprotein-I antibody
To cite this abstract in AMA style:
Pandya J, Onel K, Erkan D. The Clinical Relevance of Different Antiphospholipid Antibody Profiles in Pediatric Rheumatology Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-clinical-relevance-of-different-antiphospholipid-antibody-profiles-in-pediatric-rheumatology-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-clinical-relevance-of-different-antiphospholipid-antibody-profiles-in-pediatric-rheumatology-patients/