Session Information
Date: Monday, November 8, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Outcomes (1257–1303)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Due to the heterogeneity of systemic lupus erythematosus (SLE), clinical characteristics, quality of life (QOL), social determinant of health (SDOH), health care utilization (HRU), and cost are important metrics in evaluation of treatment efficacy. Our study sought to use a generalizable real-world data source to characterize SLE patient characteristics compared to the general population.
Methods: We analyzed 2016 – 2018 Medical Expenditure Panel Surveys (MEPS). MEPS is an annual survey designed to represent the US civilian non-institutionalized population. SLE patients were identified using ICD-10 M32 and had to have either/or SLE-related medication and rheumatologist visit. A non-SLE (referent) cohort from the general MEPS population was 1:5 matched using matching without replacement to SLE patients on index year, age, gender, and geographic region. Data were pooled across all three years. Continuous variables and proportions were compared with t-tests or Chi-square tests, respectively. Logistic models were used to evaluate the odds ratio (OR) of SLE vs controls for HRU and QOL outcomes. Generalized linear models (GLM) were used to assess mean cost differences comparing adults with SLE to controls. The 95% confidence intervals (CI) were reported for all models adjusted for race, payer, and key comorbidities.
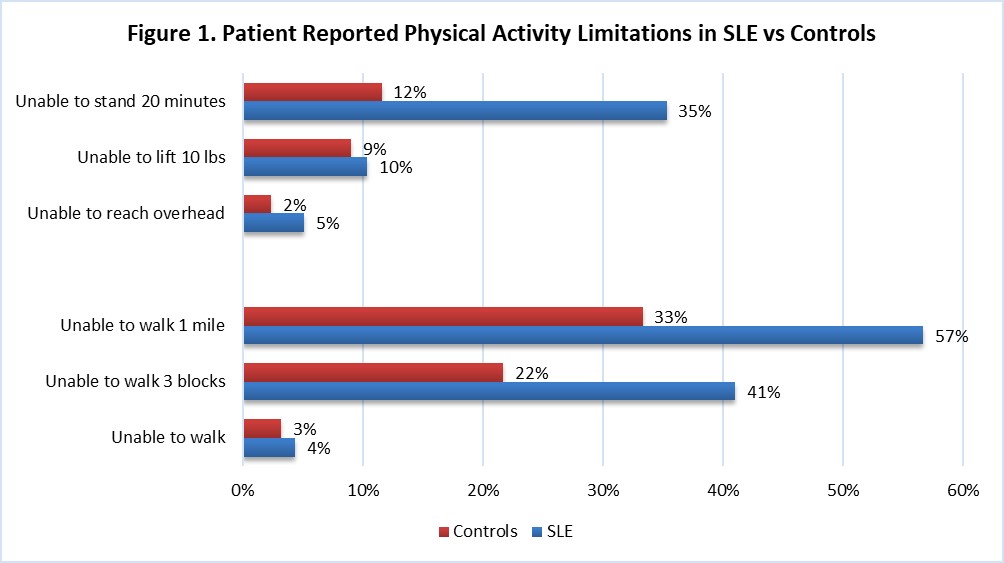
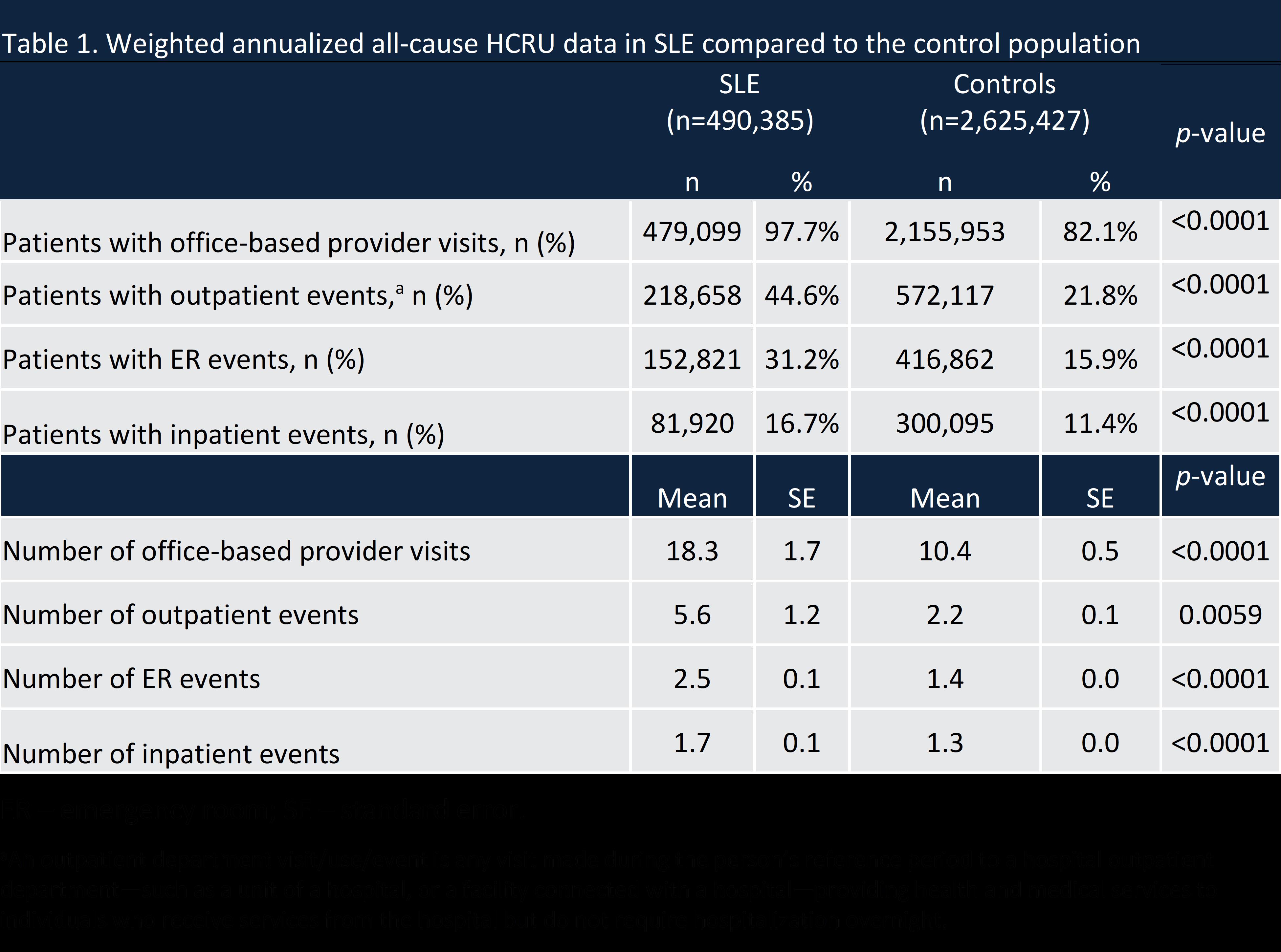
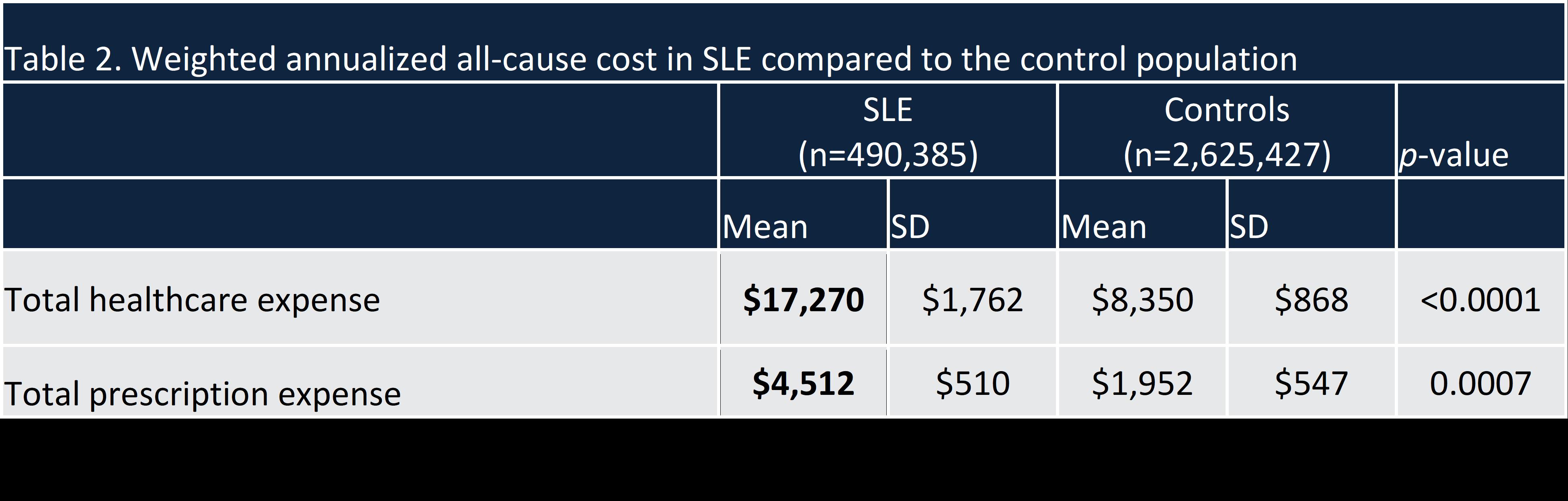
Results: 154 (0.16%) respondents among 96,996 adults who reported annual data in MEPS met our criteria for SLE. After applying weights to generate nationally representative estimates, SLE adults were more likely to be publicly insured (35% vs. 18%), have lower median family income ($46,925 vs. $70,624), and higher unemployment (50% vs. 34%); however, education level did not differ compared to the non-SLE cohort. Comorbidities were significantly higher in SLE vs. non-SLE adults, including joint pain (63% vs. 33%), arthritis (61% vs 29%), hypertension (39% vs 26%), asthma (27% vs. 13%) and heart disease (24% vs. 8%). 17% percent of SLE respondents reported they were “unable to work due to illness/disabled” compared to only 3% of non-SLE adults. More SLE adults reported “delaying getting necessary care” (14% vs. 5%) and “unable to pay family medical bills” (16% vs. 5%) than the non-SLE cohort. The adjusted odds ratio of “pain limited work” was significantly higher in SLE adults vs. controls (2.5 (95% CI: 1.4,4.3)). Adults with SLE were significantly more likely to report perceived poorer physical and mental health, including a higher OR of depression (2.1 (95% CI: 1.3, 3.3)). SLE adult had a higher HRU of outpatient and ER visits with approximately twice as many annual visits. All-cause healthcare and prescription expenses were significantly higher in SLE adults compared to non-SLE patients ($17,270 vs $8,350 and $4,512 vs $1,952 respectively).
Conclusion: This study characterizes adults with SLE compared to the general non-SLE population in a nationally representative weighted data source. Overall, comorbidity, QOL, HRU and cost burden was higher in SLE compared to non-SLE adults. It is essential to understand both direct and indirect factors in HRU and cost, including patient experience, to make treatment recommendations and decrease disease burden.
To cite this abstract in AMA style:
Grabich S, Farrelly E, Ortmann R, Pollack M, Sze-jung Wu S. The Burden of Systemic Lupus Erythematosus Patients in the United States – Evidence from the Medical Expenditure Panel Survey (2016-2018) [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-burden-of-systemic-lupus-erythematosus-patients-in-the-united-states-evidence-from-the-medical-expenditure-panel-survey-2016-2018/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-burden-of-systemic-lupus-erythematosus-patients-in-the-united-states-evidence-from-the-medical-expenditure-panel-survey-2016-2018/