Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Poverty increases non-communicable disease risk, however its influence on systemic lupus erythematosus (SLE) burden is poorly understood. Non-White racial/ethnic groups, particularly of African origin, disproportionately suffer both from SLE and poverty, making disentangling racial/ethnic vs socioeconomic influences on SLE outcomes a challenge. Saint Lucia is a Caribbean island with a predominantly African ancestry population and variable socioeconomic dynamics. We therefore tested the association between poverty and SLE severity in a unique African ancestry SLE cohort.
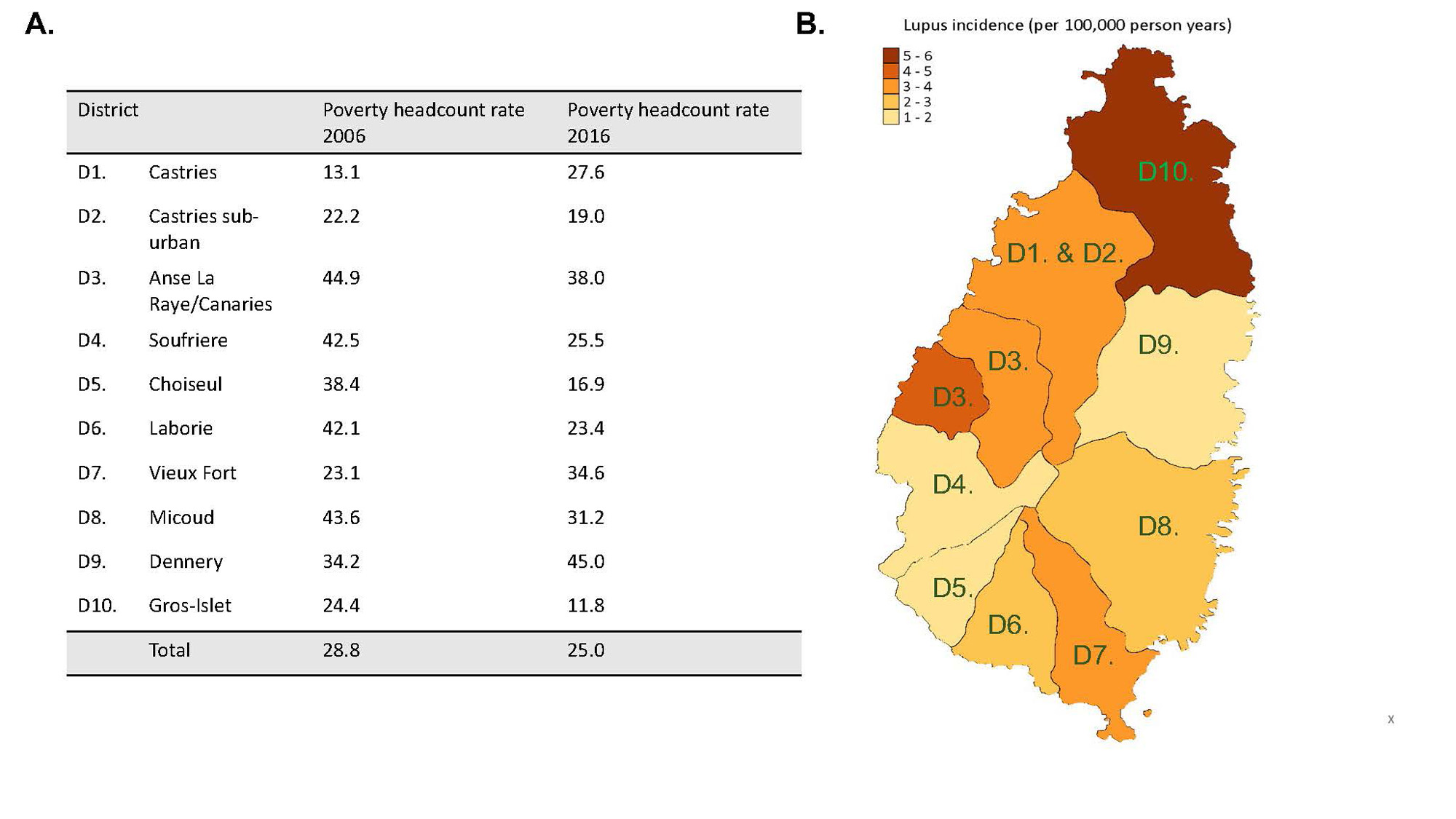
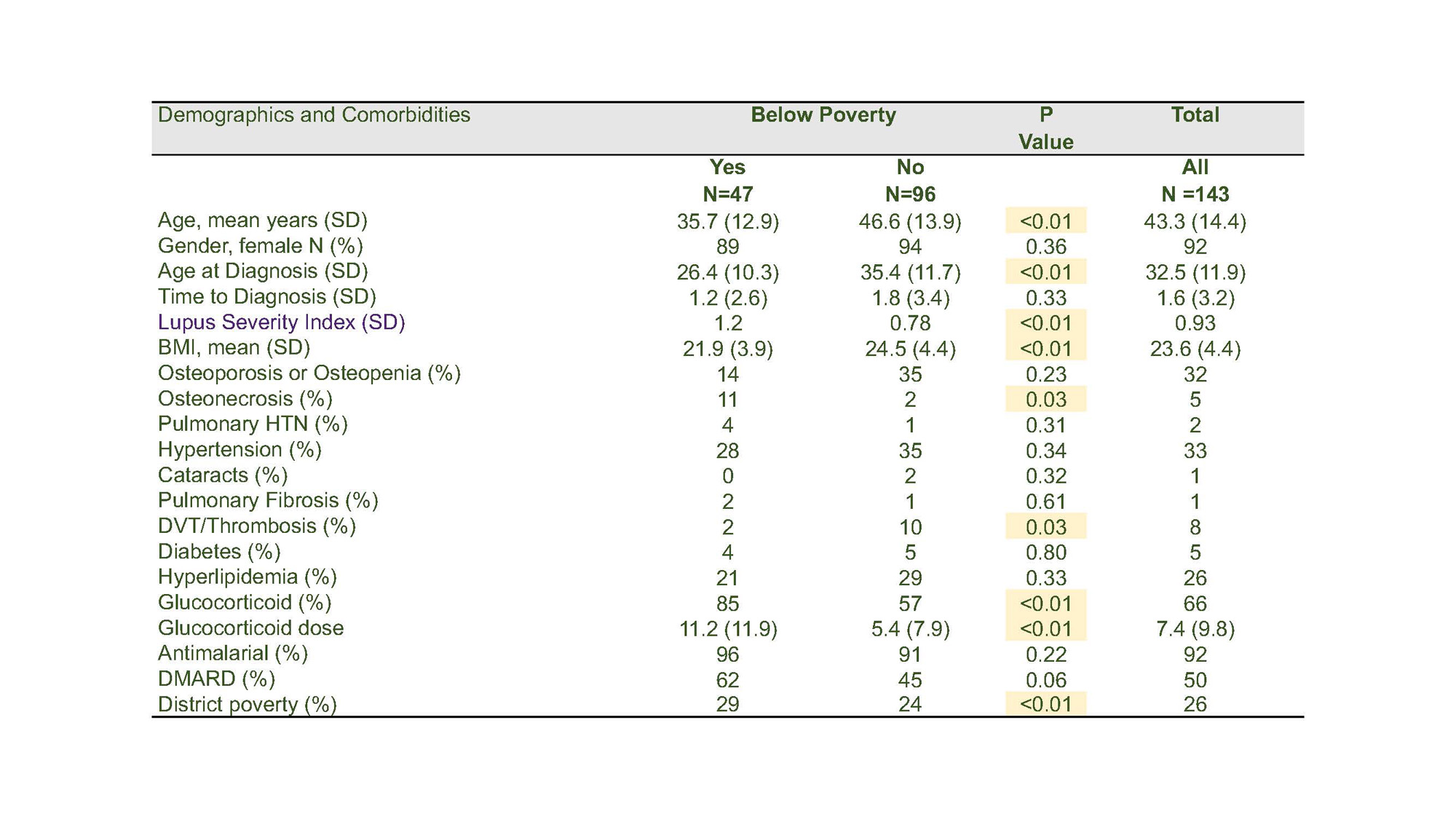
Methods: A 143-patient SLE cohort seeking care with the single practicing rheumatologist in Saint Lucia were included. All participants were at least 18 years old and met SLE classification criteria. Given that all rheumatology care is performed at this center, the cohort is expected to represent near-enumeration of SLE for the island population. Clinical data, demographics, and socioeconomic factors were obtained via chart review. Addresses identified district of residence, and area level poverty percentages in 2016 were obtained from the Saint Lucia National Report of Living Conditions. Incidence rates were calculated as the number of cases per 100,000 person-years of observation. The primary outcome was the Lupus Severity Index (LSI); calculated as a summation of ACR 1997 criteria multiplied by validated regression coefficients. Covariates that associated with LSI were identified by simple linear regression. Multiple regression was used to test the association between key covariates and LSI.
Results: The 2015-2018 incidence of SLE was 8 per 100,000 person-years (95% CI: 5.1-11.9). Incidence by district is shown in Figure 1. Of the 143 participants, 47 were below and 96 were above the poverty threshold. Impoverished patients were diagnosed 10 years earlier than non-impoverished patients, had lower BMIs, were more likely to live in impoverished districts, to take glucocorticoids at higher doses, and had higher lupus severity indexes than non-impoverished patients (table 1). Survival over the observation period was 85% in impoverished and 94% in non-impoverished participants (p=0.09). Linear regression models revealed associations between poverty status (p=0.002), younger age at onset (p=0.02), residence in an area with greater poverty level in 2016 (p=0.04), and higher glucocorticoid dose (p< 0.001), and greater LSI.
Conclusion: In this predominantly African ancestry SLE cohort, poverty associated with early onset SLE, higher Lupus Severity Index, and heavier reliance on glucocorticoid therapy. There were trends toward higher case fatality in impoverished participants. These data implicate socioeconomic stress in SLE disease burden and support further studies into the mechanis
To cite this abstract in AMA style:
King A, Brown C, Altenor C, Niewold T, Blazer A. The Association Between Poverty and SLE Disease Burden: Experiences from a Saint Lucian Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-association-between-poverty-and-sle-disease-burden-experiences-from-a-saint-lucian-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-poverty-and-sle-disease-burden-experiences-from-a-saint-lucian-cohort/