Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Non-restorative sleep is associated with poorer cognitive function and greater fatigue, not only in people living with fibromyalgia (FM), but also in the general population. Whether the extent of non-restorative sleep impacts on diurnal patterns of cognitive function and fatigue, and whether this differs based on FM status, has yet to be established.
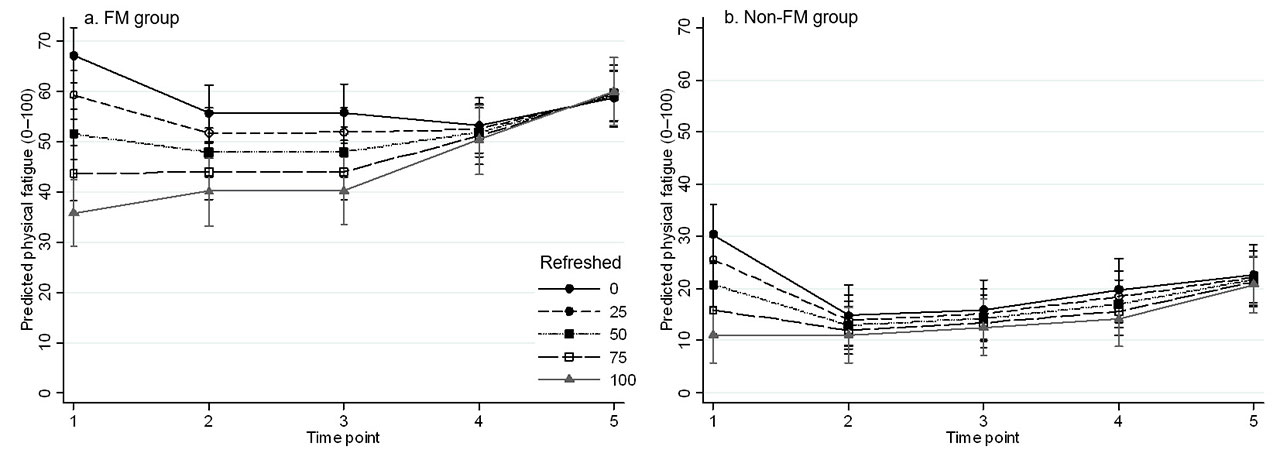
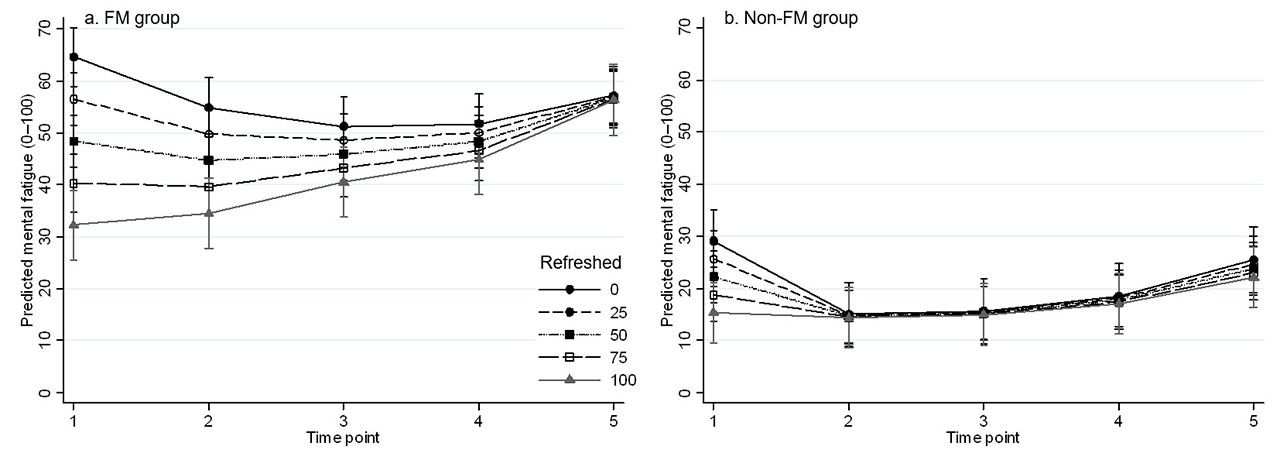
Methods: This secondary analysis used data collected from 100 participants recruited to an ambulatory study conducted in real-world settings (50 participants who met 2016 ACR FM diagnostic criteria and 50 age-, sex- and education-matched non-FM controls). Participants reported the degree to which they felt refreshed upon awakening (0–100 scale, higher scores representing more restorative sleep). Ecological momentary assessments of self-reported cognitive function (perceived clarity and speed) and mental and physical fatigue (all measured using 0–100 numeric rating scales) were administered five times per day for eight days using a smartphone app. Multilevel linear regression models were used to investigate whether perceived level of refreshment on awakening was associated with diurnal symptom patterns of cognitive function and physical and mental fatigue.
Results: Mean age of the sample was 45.1 years (SD 13.9); 88% were female. A total of 756 days of data were available for analysis. Compared to the non-FM group, the FM group reported higher aggregate levels of cognitive dysfunction (mean difference: 31.5, 95%CI 25.2–37.8), physical fatigue (mean difference: 36.3, 95%CI 29.6–43.0), and mental fatigue (mean difference: 32.0, 95%CI 24.8–39.2). For both groups, non-restorative sleep was associated with greater cognitive dysfunction and fatigue (both mental and physical) on awakening. For the FM group, the effects of non-restorative sleep were sustained across the course of the day; for the non-FM group, recovery was swift (Figures 1–3). There was a significant interaction between Group membership and impact of non-restorative sleep on diurnal symptom patterns for both physical and mental fatigue (p< 0.01), but not cognitive function (p=0.07).
Conclusion: Nights of non-restorative sleep exert negative effects on cognitive function and fatigue that persist longer into the day for those with FM compared to non-FM controls. If supported by further investigation, the diurnal patterns observed in the FM group may indicate optimal times for task planning and therapeutic engagement in response to subjective feelings of refreshment on morning awakening.
To cite this abstract in AMA style:
Whibley D, Williams D, Clauw D, Kratz A. The Association Between Non-restorative Sleep and Diurnal Patterns of Cognitive Function and Fatigue in People with Fibromyalgia and Matched Controls [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-association-between-non-restorative-sleep-and-diurnal-patterns-of-cognitive-function-and-fatigue-in-people-with-fibromyalgia-and-matched-controls/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-non-restorative-sleep-and-diurnal-patterns-of-cognitive-function-and-fatigue-in-people-with-fibromyalgia-and-matched-controls/