Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Serum titers of anti-type Ⅱ collagen (anti-CⅡ) antibodies were reported to rise at the recurrence of relapsing polychondritis (RP). It remains to be identified whether anti-CⅡ antibodies at the time of diagnosis are risk factors for relapse. The aim of this study is to investigate the association between anti-CⅡ antibodies at diagnosis and relapse.
Methods: We conducted a retrospective study of patients diagnosed with RP in our hospital between April 2006 and June 2020. Relapse was defined as aggravation of manifestations or worsening of imaging findings which require intensified treatments. Anti-CⅡ antibodies were assayed by a clinically certificated ELISA test.
Results: Eighteen patients were included in this study. The median age at diagnosis was 68.2 years (IQR 56.4-72.7 years), and 55.6% were females. The median period of observation was 40.9 months (IQR 20.7-57.1 months). Seven patients had relapses (38.9%). The median time to the first relapse was 161 days (IQR 135-394 days). The anti-CⅡ antibodies were tested in 13 patients. Tracheobronchial involvement and nasal chondritis were more frequent in the relapse group compared to the non-relapse group (71.4% vs 18.2%, p = 0.049; 85.7% vs 9.1%, p = 0.002, respectively). The relapse group had higher levels of anti-CⅡ antibodies at diagnosis [median (IQR) : 66.8 EU/mL(38.9-131.8 EU/mL) vs 14.5 EU/mL(10.7-18.7 EU/mL), p = 0.001] (Figure 1). Comparing for initial treatments, the relapse group tended to receive higher dose of prednisolone (median (IQR) 45.0mg (25.0-50.0 mg) vs 30.0mg (1.5-40.0 mg), p = 0.055). Immunosuppressive drugs and biologics were more often used in the relapse group (57.1% vs 0%, p = 0.011). Kaplan-Meier estimates of the relapse-free survival showed the anti-CⅡ antibodies positive group was significantly more likely to relapse than the negative group (Log-rank p = 0.009; HR = 1.017, 95% CI 1.004-1.031) (Figure 2).
Conclusion: High titers of anti-CⅡ antibodies at the time of diagnosis are the risk factors for relapse. This study shows that tracheobronchial involvement may also be a factor associated with relapse. We plan to measure anti-CⅡ antibodies in consistent intervals and discuss whether routine anti-CⅡ antibodies monitoring is useful for predicting future relapse.
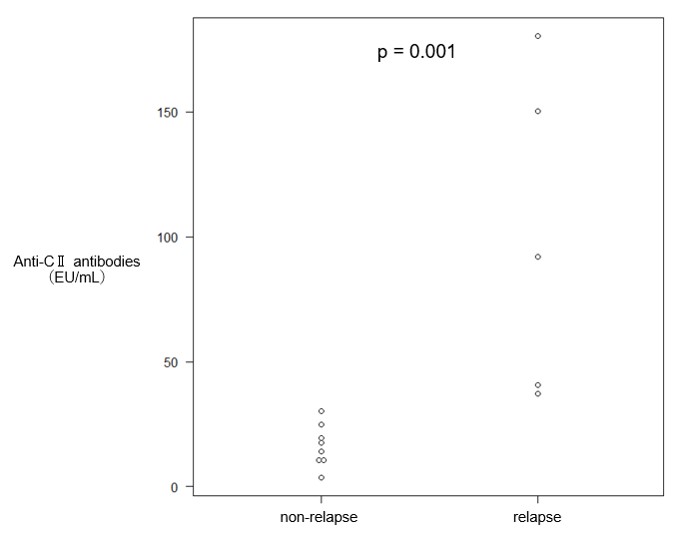 Figure1. Anti-CⅡ antibody titers of the relapse and non-relapse groups
Figure1. Anti-CⅡ antibody titers of the relapse and non-relapse groups
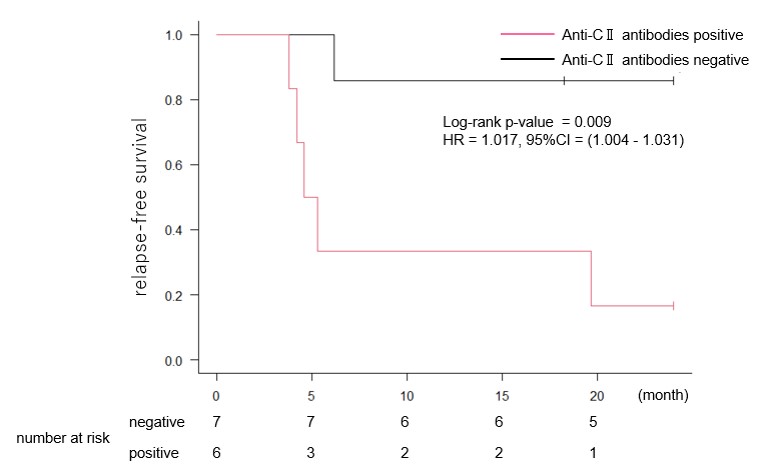 Figure 2. Kaplan-Meier survival curve for relapse in the Anti-CⅡ antibodies positive and negative groups
Figure 2. Kaplan-Meier survival curve for relapse in the Anti-CⅡ antibodies positive and negative groups
To cite this abstract in AMA style:
Iri O, Nishimura K, Waki D, Yo K, Inaba R, Yamamoto S, Mizukawa K, Yoshida T, Murabe H, Yokota T. The Association Between Anti-Type Ⅱ Collagen Antibodies at the Time of Diagnosis and Recurrence in Relapsing Polychondritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-association-between-anti-type-%e2%85%b1-collagen-antibodies-at-the-time-of-diagnosis-and-recurrence-in-relapsing-polychondritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-anti-type-%e2%85%b1-collagen-antibodies-at-the-time-of-diagnosis-and-recurrence-in-relapsing-polychondritis/
