Session Information
Date: Tuesday, October 28, 2025
Title: Abstracts: Reproductive Issues in Rheumatic Disorders (2627–2632)
Session Type: Abstract Session
Session Time: 3:45PM-4:00PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) primarily affects females of childbearing age and increases the risk of adverse pregnancy outcomes (APOs), particularly in non-White individuals and those with active disease. This study leveraged an urban multi-ethnic longitudinal SLE pregnancy cohort to evaluate predictors of APOs, with a focus on DORIS remission and outcomes across multiple pregnancies—two underexplored areas in SLE pregnancy research. The incidence of intrahepatic cholestasis of pregnancy, a rare condition not well-characterized in SLE that may increase the risk of preeclampsia, was also assessed.
Methods: The cohort includes 114 pregnancies in 95 consecutively consented SLE patients classified by ACR, SLICC and/or EULAR criteria. Clinical and laboratory data were collected during routine rheumatology visits. The primary outcome was a composite of APOs using modified PROMISSE definitions, which included preeclampsia, preterm premature rupture of membranes (PPROM), preterm birth (PTB) < 36 weeks, small for gestational age (SGA) birth, fetal death >10 weeks’ gestation, and neonatal death within 28 days of birth. Logistic regression assessed predictors including race/ethnicity, history of lupus nephritis, autoantibodies, disease activity measured by SLEPDAI, DORIS remission, and medications. For patients with >1 pregnancy, only the first was included in regression analyses; a descriptive analysis examined the impact of prior APOs on future pregnancy outcomes.
Results: Among 95 pregnant SLE patients, 28% were Hispanic, 44% White, 32% Black, and 13% Asian. APOs occurred in 57%, most commonly preeclampsia (27%), SGA < 5th percentile (20%), and PTB (18%) (Table 1A). Significant predictors included antihypertensive use (OR 10.2, p=0.029), prior lupus nephritis (OR 2.5, p=0.034), non-White race (OR 2.4, p=0.039), Black race (OR 2.8, p=0.003), higher SLEPDAI (OR 1.11, p=0.022), and anti-Sm positivity (OR 3.3, p=0.01) (Table 2). LAC was associated with neonatal death. All APOs occurred with higher frequency in those who were not in sustained DORIS remission and significantly associated with PTB and preeclampsia (Tables 1B, 2). Notably, all 4 neonatal deaths occurred in patients not in DORIS remission. In the 16 patients with multiple pregnancies, the proportion in DORIS remission improved from 62% in the first pregnancy to 81% in the second pregnancy. While 8 of these 16 (50%) had an APO in the first pregnancy, only 3 had recurrent APOs, and 1 developed a new APO in pregnancy 2 (Figure 1A-B). Compared to the reported frequency of intrahepatic cholestasis in 0.2 to 2% percent of healthy pregnancies, it occurred in 8/114 pregnancies (7%, one patient twice, one with APO).
Conclusion: In this diverse SLE cohort, known predictors of APOs – including antihypertensive use, prior nephritis and active disease – were confirmed. The absence of DORIS remission was associated with preeclampsia and PTB. Prior pregnancy morbidity did not predict future APOs. These findings highlight the relevance of DORIS remission to maternal-fetal outcomes. The high prevalence (7%) of cholestasis of pregnancy in this cohort warrants further attention given its known fetal risks.
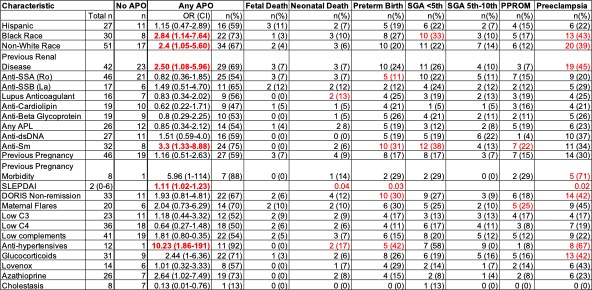 Table 1. Characteristics and Outcomes in the Pregnancy Cohort. A. N is specified where it differs from the overall sample size. Data is represented as N (%) for categorical variables and median (IQR) for continuous variables. *Low complements, thrombocytopenia, anti-dsDNA (crithidia), DORIS, and cholestasis were considered if present at any time during pregnancy. **The highest SELENA SLEPDAI during pregnancy is represented as well as the measure taken during each trimester. Medications include those taken at any time during pregnancy. B. Pregnancy outcomes in the SLE cohort (Nf95), also stratified by DORIS remission status.
Table 1. Characteristics and Outcomes in the Pregnancy Cohort. A. N is specified where it differs from the overall sample size. Data is represented as N (%) for categorical variables and median (IQR) for continuous variables. *Low complements, thrombocytopenia, anti-dsDNA (crithidia), DORIS, and cholestasis were considered if present at any time during pregnancy. **The highest SELENA SLEPDAI during pregnancy is represented as well as the measure taken during each trimester. Medications include those taken at any time during pregnancy. B. Pregnancy outcomes in the SLE cohort (Nf95), also stratified by DORIS remission status.
.jpg) Table 2. Predictors of Adverse Pregnancy Outcome. Characteristics of interest are shown in the left most column. The proportion of patients with each characteristic who had the defined APOs is represented. A logistic regression analysis was used to associate each characteristic with APOs. Significant associations are highlighted in red.
Table 2. Predictors of Adverse Pregnancy Outcome. Characteristics of interest are shown in the left most column. The proportion of patients with each characteristic who had the defined APOs is represented. A logistic regression analysis was used to associate each characteristic with APOs. Significant associations are highlighted in red.
.jpg) Figure 1: A. Table describing the characteristics of patients with multiple pregnancies. B. Map showing the pregnancy outcomes and DORIS remission of 16 patients with multiple pregnancies in the lupus pregnancy cohort. Pink colored boxes indicate the presence of that outcome. Grey boxes indicate the absence of that outcome. Only 3 patients had a third pregnancy represented.
Figure 1: A. Table describing the characteristics of patients with multiple pregnancies. B. Map showing the pregnancy outcomes and DORIS remission of 16 patients with multiple pregnancies in the lupus pregnancy cohort. Pink colored boxes indicate the presence of that outcome. Grey boxes indicate the absence of that outcome. Only 3 patients had a third pregnancy represented.
To cite this abstract in AMA style:
Hernández-Blanco C, Carlucci P, Izmirly P, Dai J, Masson M, Belmont M, Saxena A, Salmon J, Brandt J, Buyon J. The Absence of DORIS Remission Is Associated with Greater Risk of Preterm Birth and Preeclampsia in SLE Pregnancies [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-absence-of-doris-remission-is-associated-with-greater-risk-of-preterm-birth-and-preeclampsia-in-sle-pregnancies/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-absence-of-doris-remission-is-associated-with-greater-risk-of-preterm-birth-and-preeclampsia-in-sle-pregnancies/
