Session Information
Date: Monday, November 9, 2015
Title: Health Services Research II: Rheumatoid Arthritis Treatment and Healthcare Utilization
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Monitoring of drug use and
costs can: describe trends in expenditures over time, identify regional
variations in access and indicate physicians’ uptake of best-practice guidelines.
Our aim was to describe drug use and costs of biologic (bDMARD)
and conventional synthetic Disease Modifying
Anti-Rheumatic drug (csDMARDs) in the context
of single-payer universal drug coverage.
Methods: We performed a population-based analysis,
identifying all RA patients (from 1995 to 2013) who were aged 65 years and
older using a validated algorithm (1) (n=37,012). All patients received
identical public drug coverage from a single public payer. Prescriptions were
determined using the pharmacy claims database of the Ontario Drug Benefit
Program. For each patient we recorded the annual
number of prescriptions and costs for csDMARDs and bDMARDs and region of residence. Trends
in annual drug use and costs were graphed by drug class and regional health
authority.
Results: The total number of patients receiving RA
medications tripled from 14,222 in 1995 to 37,012 in 2013. During that same
time period csDMARD use and costs increased from
$2.1M in 1995 to $8.5M in 2013(Fig 1.). When bDMARDs
were introduced in 2001, 105 patients received bDMARDs
(0.4%) increasing to 3226 patients (11%) in 2013. During that period the costs
of bDMARDS increased from $0.78M to $54.6M (Fig
1.).
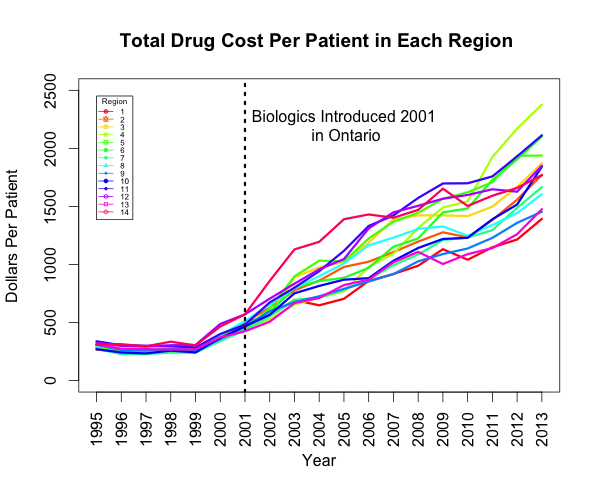
In 1995, per-patient drug
costs in each regional health authority were an average of $500 per patient per
year(Fig 2.). Since the introduction of bDMARDs in 2001, total cost and per-patient cost variation
among regions has increased considerably, with drug expenditure in 2013 ranging
from $1200 per patient per year to $2500 per patient per year(Fig
2.).
Conclusion: The number of patients with RA increased
linearly over time from 1995 to 2013. The proportion of patients receiving csDMARDs grew at the same rate as the population of
patients with RA. The introduction of bDMARDs was
associated with an exponential rise of bDMARD use and
cost over time driving the increase in total drug costs however the use of bDMARDs was lower than in the US where 27% of patients with
a mean age of 70 received bDMARDs (2).
When analyzed by region, adoption of bDMARDs
was associated with differential and widening variation in regional drug costs
over time, indicating unequal use of bDMARD not
explained by differences in reimbursement criteria. We hypothesize that
regional access to rheumatology care and rheumatologist’s varying propensity to
prescribe bDMARDs are the
primary drivers of inequitable utilization of bDMARDs.
References
1. Widdifield
et al. , Arthritis Care Res, 2013.
2. Zhang et
al., Arthritis Care Res, 2013.x
To cite this abstract in AMA style:
Tatangelo M, Paterson M, Tomlinson GA, Bansback N, Widdifield J, Gomes T, Bombardier C. Temporal Trends in Drug Prescription, Utilization and Costs Among Rheumatoid Arthritis (RA) Patients Show Wide Regional Variation Despite Universal Drug Coverage [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/temporal-trends-in-drug-prescription-utilization-and-costs-among-rheumatoid-arthritis-ra-patients-show-wide-regional-variation-despite-universal-drug-coverage/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/temporal-trends-in-drug-prescription-utilization-and-costs-among-rheumatoid-arthritis-ra-patients-show-wide-regional-variation-despite-universal-drug-coverage/