Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Exercise is strongly recommended treatments to address pain and functional limitation for adults with Knee Osteoarthritis (OA) and Physical Therapy (PT) is responsible for prescribing and delivering exercise to patients. Physical activity, which includes free-living unstructured activities that are not part of formal exercise, also benefits adults with knee OA. Specifically, Moderate-to-Vigorous Physical Activity (MVPA) improves pain and functional limitation and there is a need to increase MVPA since fewer than 13% meet the 2018 Physical Activity Guidelines for Americans. Thus, we investigated if adding step goals to an established 12-week PT intervention of strength training and education increases MVPA. We also investigated changes in light intensity physical activity and steps/day as secondary outcomes, and pain and function as tertiary outcomes over 12 and 24 weeks.
Methods: We conducted an assessor-masked superiority randomized controlled trial with two parallel arms. Participants were recruited via Facebook advertisements. Those who met the National Institute for Health and Care Excellence (NICE) OA clinical criteria and reside in the contiguous US were enrolled in the trial. The intervention included five video conferencing consultations with a physical therapist over 12 weeks for strengthening exercises, steps/day goals, and education. The control intervention was a website with OA treatment resources. MVPA, light intensity physical activity and steps/day were measured with a waist-worn ActiGraph monitor over 7 days. Pain was measured with a Visual Analogue Scale [VAS] and the pain subscale of the Knee Injury and Osteoarthritis Outcome (KOOS). Function was measured with the KOOS ADL subscale. Analyses were performed using intention-to-treat methods and differences between the Intervention and control groups over three time points: baseline, 12, and 24 weeks calculated using a 2×3 between/within mixed ANOVA.
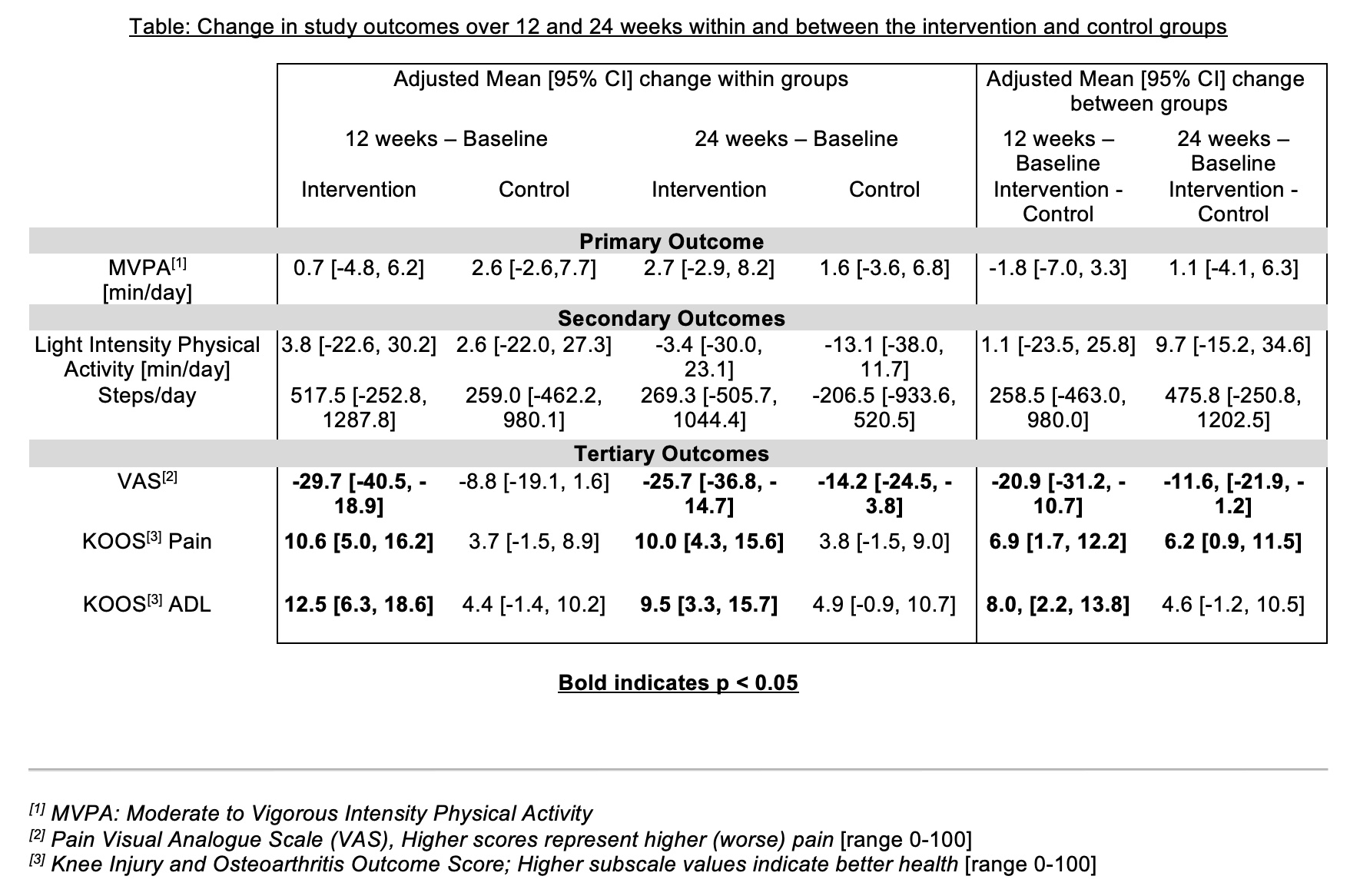
Results: Time spent in MVPA was available for n=88 study participants at baseline, 76.1% (67/88) at 12 weeks and 73.9% (65/88) at 24 weeks. Intervention participants had little change in MVPA over 12 weeks (see Table, 0.7 min/day, 95%CI [-4.8, 6.2]) which was not different than the control (between group difference -1.8 min/day [-7.0, 3.3]). Similarly, there was little change in light intensity physical activity and steps/day between groups. Tertiary outcomes were available in n=103 at baseline, 81.5% (84/103) at 12 weeks, and 80.6% (83/103) at 24 weeks. The intervention group had greater improvements on VAS pain at 12 and 24 weeks (-20.9 [-32.2, -10.7] and -11.6 [-21.9, -1.2), respectively), KOOS Pain at 12 and 24 weeks (6.9 [1.7, 12.2] and 6.2 [0.9, 11.5), respectively), and KOOS ADL at 12 weeks (8.0 [2.2, 13.8]) compared to the control.
Conclusion: Adding step goals to an established 12-week PT intervention of strength training and education did not increase MVPA in adults knee OA. This could be because there was a mismatch between the focus of the intervention, which was to increase steps/day, and the primary study outcome, time spent in MVPA. The intervention group did show improvements in pain and function compared to the control group.
To cite this abstract in AMA style:
White D, Hinman R, Videtich Bye T, Liles S, Voinier D, Copson J, Schmitt L, Bodt B, Jakiela J. Telehealth Physical Therapy Intervention to Increase Physical Activity in Adults with Knee OA: The Delaware PEAK Randomized Controlled Trial [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/telehealth-physical-therapy-intervention-to-increase-physical-activity-in-adults-with-knee-oa-the-delaware-peak-randomized-controlled-trial/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/telehealth-physical-therapy-intervention-to-increase-physical-activity-in-adults-with-knee-oa-the-delaware-peak-randomized-controlled-trial/