Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Cellular exhaustion is a cellular dysfunction characterized by the progressive loss of the effector function, and an increased expression of multiple inhibitory receptors. Exhaustion develops after repetitive stimulation and a high antigenic load. Remission in SLE can be defined as the lack of clinical and serological activity for a specific period, and it has been associated with less accrual damage, and number and severity of flares. Cellular exhaustion has been associated with a better outcome in autoimmune diseases, such as SLE and antibody associated vasculitis.
To identify exhausted CD8+ T-cells populations in prolonged remission SLE patients, active SLE patients, and in healthy subjects.
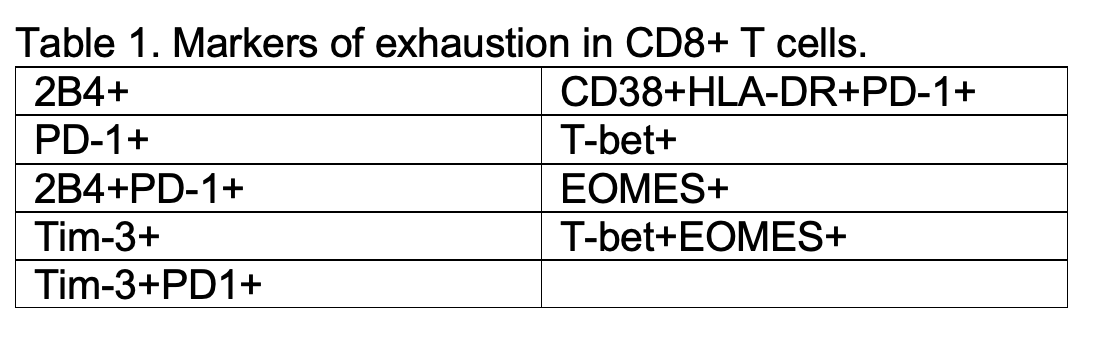
Methods: We performed a transversal exploratory study. We included patients classified with SLE according to the revised SLE ACR 1997 and SLICC 2012 criteria. Three groups were studied: 1. Prolonged remission SLE (PR SLE): patients with SLE in clinical remission of the disease, defined as a SLEDAI-2K of 0 (excluding hypocomplementemia and high anti-DNA titers), and absence of corticosteroid or immunosuppressant treatment for at least 10 continuous years. 2. Active SLE: patients with SLE with clinical activity measured with SLEDAI-2K. 3. Healthy controls: paired by gender and age ± 5 years with PR SLE group. Flow cytometry was performed to measure the expression of surface and intracellular markers associated to exhausted T CD8+ lymphocytes (Table 1). Percentage of T cells was determined using FlowJo software v10. Leukocyte counts and percent lymphocytes were used to determine the absolute lymphocytes subset counts (cells/µL) of the different subpopulations. Descriptive statistics and multiple comparisons were performed between groups.
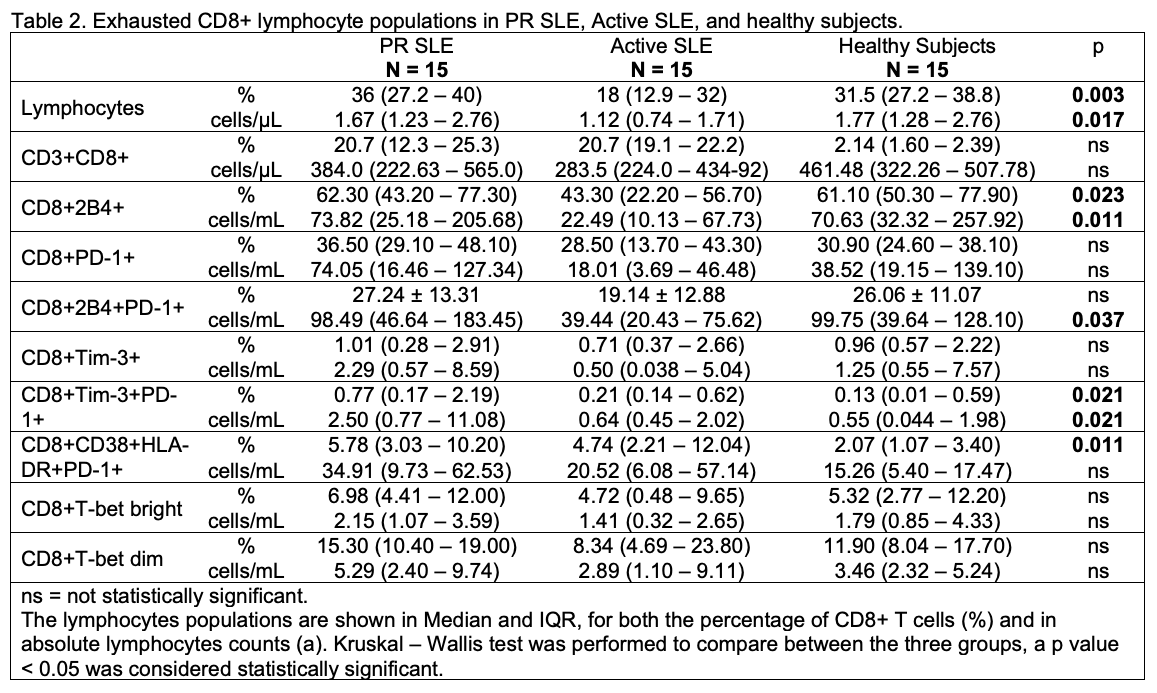
Results: We included 15 patients in each group, with an age of 49 years (48 – 60) in the PR SLE patients, 33 (30 – 46) in active SLE, and 47 (44 – 48) in healthy controls. No difference was found between age of PR SLE and healthy controls. In PR SLE patients, disease duration of SLE was 308 (230 – 425) months, and in active SLE 111 (69 – 161) months. Duration of remission state in PR SLE was 203 (146 – 248) months. The exhausted CD8+ lymphocytes analysis between groups is shown in table 2. Comparing PR SLE patients with active SLE patients with Mann Whitney U test, differences were found in CD8+2B4+ % (p = 0.049), CD8+2B4+ a (p = 0.014), CD8+2B4+PD-1+ a (p = 0.012), CD8+PD-1+ a (p = 0.040), CD8+Tim-3+PD-1+ a (p = 0.023), CD8+T-bet+ % (PR SLE 65.4 [33.3 – 71.7] vs Active SLE 28.1 [10.7 – 59.2], p = 0.010), CD8+EOMES+ % (PR SLE 42.9 [21.1 – 68.5] vs Active SLE 13.9 [10.5 – 37.2], p = 0.029), CD8+EOMES+ a (PR SLE 111.6 [58.3 – 321.4] vs Active SLE 46.2 [22.3 – 133.7], p = 0.024), CD8+T-bet+EOMES+ % (PR SLE 25.0 [18.9 – 47.6] vs Active SLE 9.86 [4.44 – 20.7], p = 0.010), and CD8+T-bet+EOMES+ a (PR SLE 93.4 [48.1 – 161.7] vs Active SLE 24.3 [8.1 – 92.3], p = 0.014).
Conclusion: SLE patients in prolonged remission express more exhausted CD8+ T cells than patients with active SLE. These findings support that cellular exhaustion is inherent to a better clinical outcome.
To cite this abstract in AMA style:
Treviño-Tello F, Lima G, Jakez-Ocampo J, Llorente L, Atisha-Fregoso Y, Fragoso-Loyo H. T-cell Exhaustion in Prolonged Remission SLE Patients [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/t-cell-exhaustion-in-prolonged-remission-sle-patients/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/t-cell-exhaustion-in-prolonged-remission-sle-patients/