Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a heterogeneous disease with patients often presenting with non-specific symptoms that can cause delays in diagnosis. Phenotype risk scores measure the degree to which a patient’s symptoms, as assessed by billing codes, overlap with defined disease criteria. Phenotype risk scores have identified patients with unrecognized Mendelian genetic disorders successfully and may help identify patients earlier with rare diseases. We developed and validated a phenotype risk score for SLE in a large electronic health record (EHR) cohort using billing codes to capture SLE criteria
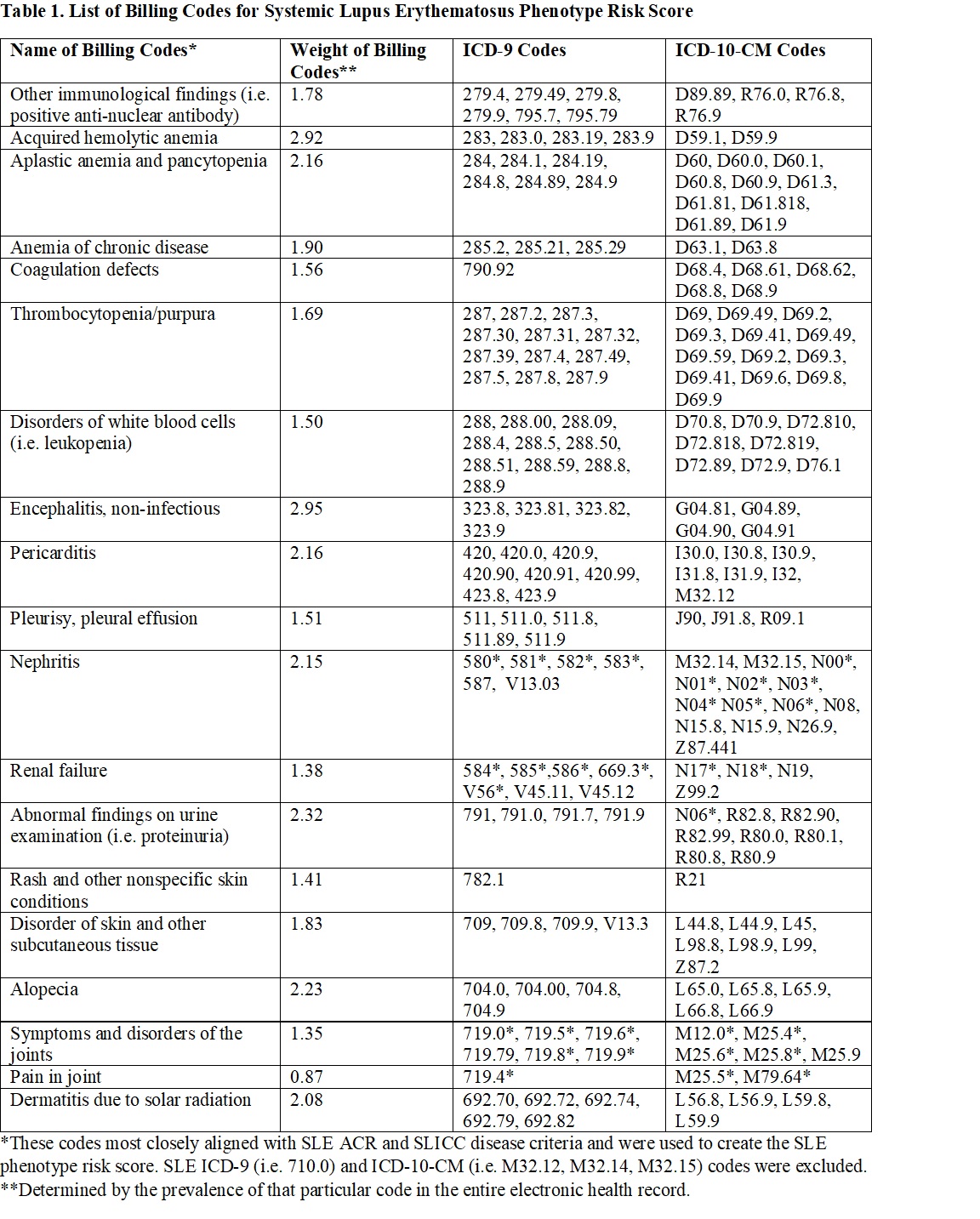
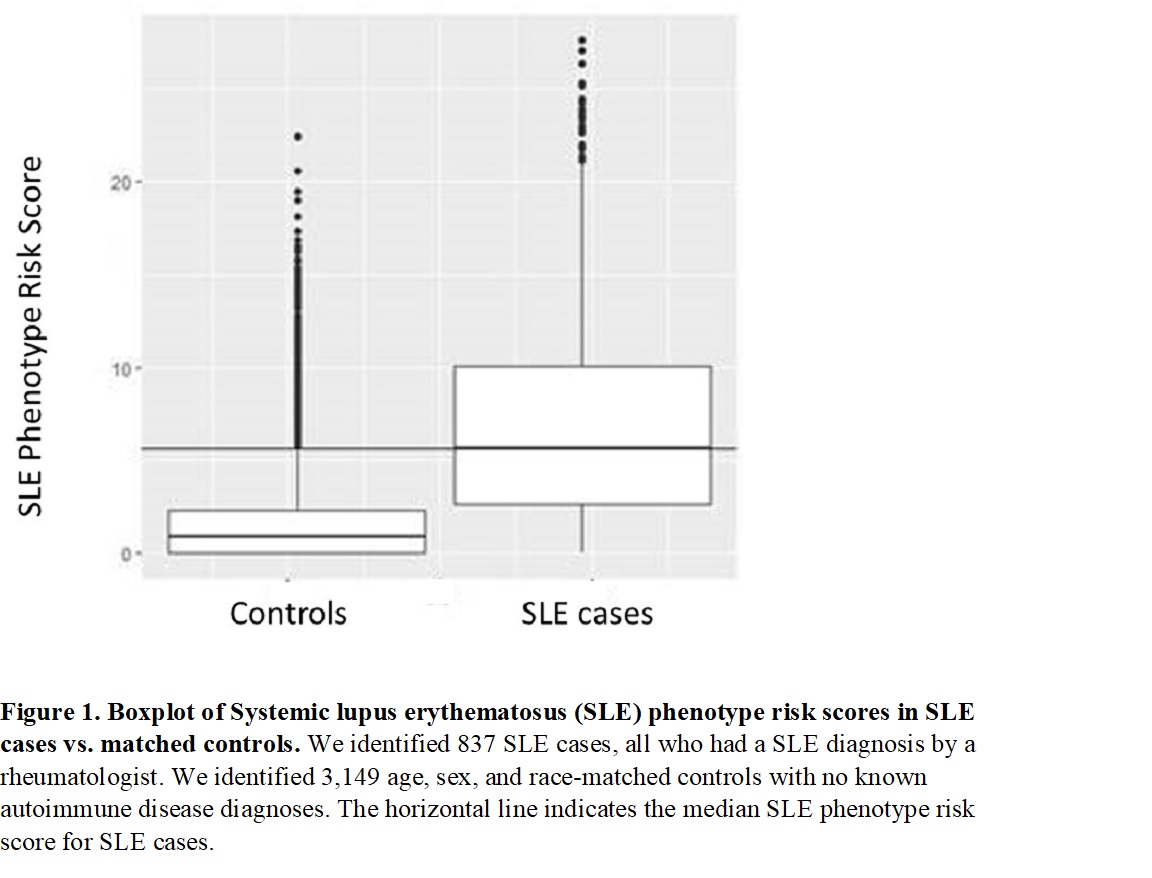
Methods: We identified 837 SLE cases from a de-identified EHR with over 3 million subjects with decades of follow-up using a previously validated and published algorithm. Subjects were required to have a SLE diagnosis by a rheumatologist. We identified 3,149 age, sex, and race-matched controls with no known autoimmune disease diagnoses. Billing codes that correspond to SLE disease criteria were used in the phenotype risk score (Table 1). The SLE phenotype risk score was the sum of these codes in a given patient weighted by the log inverse prevalence of that code in the entire EHR. Billing codes specifically for SLE (i.e. 710.0 and M32*) were excluded. We compared phenotype risk scores in SLE cases vs. matched controls and evaluated phenotype risk scores in different SLE subgroups. Chart review was conducted on 50 of the controls with the highest SLE phenotype risk scores. We performed logistic regression to estimate the association of SLE case status with phenotype risk score adjusting for demographics. Lastly, we examined phenotype risk scores over time in SLE cases.
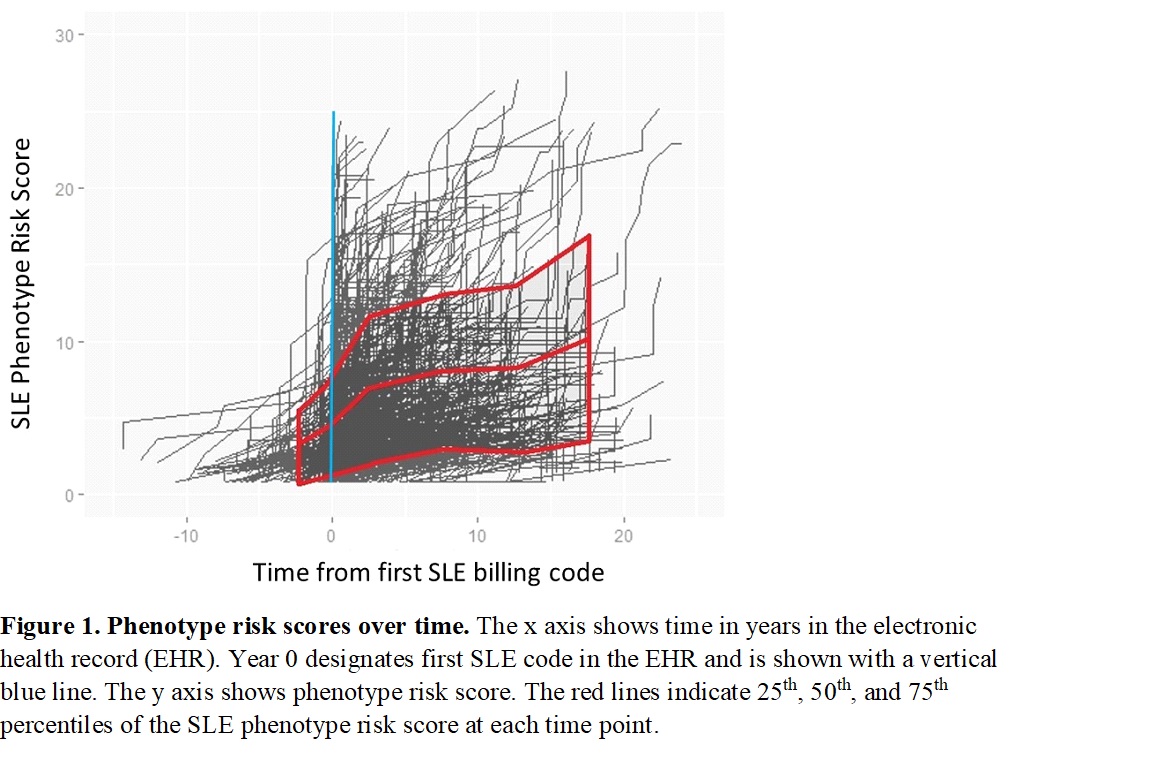
Results: SLE cases had a significantly higher SLE phenotype risk score compared to controls (7.2 ± 5.6 vs. 1.7 ± 2.5, p < 0.001) (Figure 1). The SLE phenotype risk score was significantly associated with case status after adjusting for age, sex, and race (p < 0.001). Of the 50 controls with the highest phenotype risk score, the two controls with the highest score had SLE by ACR SLE and SLICC criteria with an additional 4 patients having incomplete or probable SLE and another 8 having other autoimmune diseases including discoid lupus, Crohn’s, and inflammatory arthritis. Comparing subgroups of SLE patients, females and males had similar scores (7.1 ± 5.6 vs. 7.3 ± 5.3, p = 0.75). African Americans with SLE had significantly higher scores compared to Caucasians (9.6 ± 6.7 vs. 6.4 ± 5.0, p < 0.001). Figure 2 shows trends of SLE phenotype risk scores over time. There was a small cluster of 57 SLE patients who had phenotype risk scores ≥ 50th percentile before their first SLE billing code.
Conclusion: Due to its heterogeneity, SLE can be a difficult disease to diagnose leading to delays in diagnosis and treatment that impact patient morbidity and mortality. We developed a SLE phenotype risk score in a large EHR cohort that identifies missed SLE diagnoses. We propose that phenotype risk scores could serve as a clinical tool, potentially coupled with genetic data, to make earlier and more accurate SLE diagnoses.
To cite this abstract in AMA style:
Barnado A, Carroll R, Wheless L. Systemic Lupus Erythematosus Phenotype Risk Score Identifies Undiagnosed Cases in a Large Electronic Health Record [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/systemic-lupus-erythematosus-phenotype-risk-score-identifies-undiagnosed-cases-in-a-large-electronic-health-record/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-lupus-erythematosus-phenotype-risk-score-identifies-undiagnosed-cases-in-a-large-electronic-health-record/