Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatoid arthritis (RA) has a ‘pre-RA’ period definable as elevations of antibodies to citrullinated protein antibodies (ACPA) before clinically-apparent inflammatory arthritis (IA). ACPA elevations can predict future IA; however, most prospective studies have studied symptomatic ACPA+ individuals. As such, it is unclear how ACPA may relate to future IA in asymptomatic individuals. Furthermore, there is limited understanding of the trajectory of symptoms prior to a transition to IA, or how individuals who are prospectively followed to IA may compare with individuals with new RA found through standard rheumatology referrals.
Methods: Through clinics and screening of relatives of patients with RA and health fairs we identified 86 ACPA(+) individuals (CCP3, Inova) who had no history or examination evidence of IA. They were followed prospectively for IA development. We also evaluated 57 CCP3+ patients with EarlyRA from clinics with a baseline study visit < 30 days since confirmation of IA by a rheumatologist. Joint symptoms were captured by questionnaires capturing pain, stiffness and swelling in 68 joints. We evaluated trajectories of joint symptoms, physical examination and disease activity (DAS28CRP) through incident IA, and between individuals who transitioned to IA compared to patients with established EarlyRA.
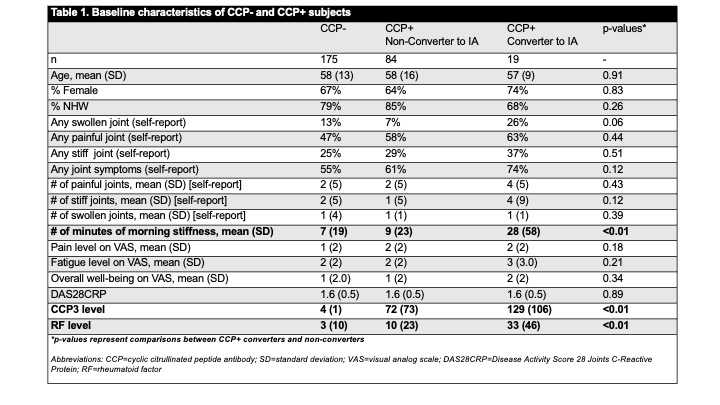
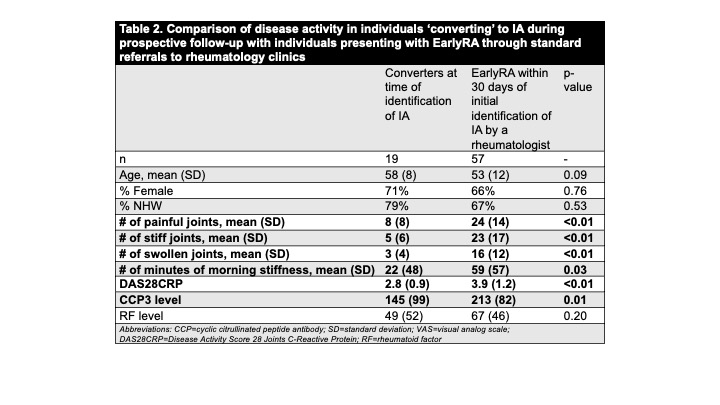
Results: Nineteen of 86 (22%) of anti-CCP3+ developed IA (‘converters’) at a median of 509 days of follow-up and 79% met 2010 ACR/EULAR criteria at time IA identification. At baseline, CCP3+ converters reported longer duration of morning stiffness, and a trend towards an increased prevalence of swollen joints compared to CCP3+ subjects who did not develop IA; in addition converters had higher levels of CCP3 and RFIgM (Table 1). In the converters there were 2 trajectories of symptoms prior to IA: 1) waxing and waning of joint symptoms and 2) period of minimal symptoms followed by steady worsening of symptoms over < 200 days prior to IA identification (these trajectories were not different than those who did not develop IA). In the ‘converters’, those without any joint symptoms at baseline (n=5) trended towards a longer duration to appearance of IA compared to those with baseline symptoms (median of 686 days vs 363 days, p~0.09). At the time of diagnosis of IA ‘converters’ had lower levels of symptoms, DAS28CRP and CCP3 than patients with EarlyRA (Table 2).
Conclusion: In this study, in CCP3+ individuals, self-reported morning stiffness and higher levels of CCP3 and RFIgM were associated with incident IA; in addition, there are 2 types of trajectories of joint symptoms in transition to IA, and a subset of CCP3+ individuals without symptoms developed IA. These findings can be considered in understanding the natural history of RA and building prediction models for future disease as well as to correlate biomarker changes with symptoms. Furthermore, the lower disease activity in ‘converters’ to IA compared to EarlyRA could indicate that prospective follow-up of ACPA+ individuals can identify IA at a time point where disease activity and CCP3 levels are less than in standard referral patterns, perhaps indicating a stage of disease more responsive to therapy.
To cite this abstract in AMA style:
Haville S, Seifert J, Barzideh S, Moss L, Rao N, Johnsen A, Buckner J, James E, Posso S, Firestein G, Boyle D, Robinson W, Holers V, Deane K. Symptom Trajectories in the Transition from Pre-Rheumatoid Arthritis to Clinically-Apparent Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/symptom-trajectories-in-the-transition-from-pre-rheumatoid-arthritis-to-clinically-apparent-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/symptom-trajectories-in-the-transition-from-pre-rheumatoid-arthritis-to-clinically-apparent-inflammatory-arthritis/