Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: The current dominant hypothesis explains fibromyalgia (FM) as a centralized pain state in which the CNS originates or amplifies pain, which is then accompanied by fatigue, memory problems, and sleep and mood disturbances1. The often noted “pan-positive review of symptoms” is attributed to central hyperresponsiveness not to psychological factors or “somatization.”1 Surprisingly, this explanation of non-pain symptoms has never been validated. As fibromyalgia and widespread pain (WP) have been accepted as evidence of the presence of central sensitization (CS), we used the widespread pain index (WPI), a non-symptom containing component of the polysymptomatic distress scale (PSD), to test whether the rate of increase in non pain symptoms as WP increased was greater in the presence of PSD defined fibromyalgia and WSP then in their absence.
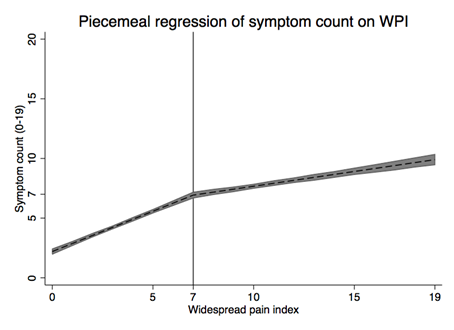
Methods: We studied 3,562 mixed rheumatic disease patients, and diagnosed FM by modified ACR FM criteria. To preclude bias because of the non-pain symptoms included in the PSD, we used WPI alone and as a surrogate for the PSD. We formed an ad hoc fibromyalgia symptom count (FSC) (0-19) by summing 19 non-pain related symptoms. We used linear splines and regression models to calculate separate slopes for symptom prediction at WPI levels between 0-6 and 7-19. An increase in the slope of the 7-19 WPI scores compared with the 0-6 WPI scores was accepted as evidence of the effect of CS.
Results: 96% of those with a WPI score ≥7 satisfied WP criteria, and FM was correctly classified in 89% (kappa 0.703). The FSC increased monotonically as WPI increased (Figure 1), and the slope for WPI 0-6 was 0.68 compared with 0.25 for 7-12 (P<0.001). For each of the 19 symptoms examined, slopes were compared by odds ratios and were significantly lower in the 7-12 group (Table 1).
Conclusion: Our data show no increase in non-pain symptom slopes in subjects with high WPI. Instead, symptom increase is monotonic, and the rate of increase is greater at lower levels of WPI. Alternative hypotheses for increase in symptoms should include factors such non-CS pain and psychological variables.
References 1. Clauw DJ. Fibromyalgia: A Clinical Review. JAMA. 2014;311(15):1547-1555.
Table 1. Odds ratios (OR) for rate of symptoms in WPI ≥7 compared with 0-6
|
Variable |
OR |
Variable |
OR |
Variable |
OR |
|
Diarrhea |
0.85 |
Nausea |
0.79 |
Tinnitus |
0.90 |
|
Dizziness |
0.83 |
Paresthesias |
0.81 |
Vision prob
|
0.83 |
|
Dry eyes |
0.88 |
Photosensitivity |
0.86 |
Vomiting |
0.87 |
|
Dry mouth |
0.85 |
Bruising |
0.82 |
Alopecia |
0.89 |
|
Dyspnea |
0.88 |
Heartburn |
0.85 |
Anorexia |
0.83 |
|
Hearing prob
|
0.87 |
Rash |
0.92* |
Asthma |
|
|
Urticaria |
0.83 |
Reynaud’s |
0.91 |
Constipation |
0.84 |
|
Oral ulcer |
0.84 |
Seizures |
0.89* |
Fever |
0.84 |
|
Muscle weakness |
0.77 |
Dysgeusia |
0.82 |
Itching |
0.86 |
*Not significant
Disclosure:
F. Wolfe,
None;
B. T. Walitt,
None;
J. Rasker,
None;
R. S. Katz,
None;
W. Häuser,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/symptom-increase-in-fibromyalgia-is-not-consistent-with-the-central-sensitization-or-central-hyperresponsiveness-hypothesis/