Session Information
Date: Sunday, October 26, 2025
Title: (0671–0710) Systemic Sclerosis & Related Disorders – Clinical Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Virtually all patients with systemic sclerosis (SSc) experience gastrointestinal (GI) manifestations over the course of their disease, affecting any region from the mouth to the anorectum. Currently, there are limited risk factors predicting worse GI outcomes in patients with early SSc. In this study, we aimed to use baseline GI symptoms to better characterize the clinical heterogeneity and outcomes in SSc-related GI disease.
Methods: Patients with SSc who were enrolled in our large, well-defined prospective cohort were included in the study. All participants met the 2013 ACR/European League Against Rheumatism classification criteria and had a disease duration of less than five years from the onset of their first non-Raynaud’s symptom at the time of enrollment. They were followed every six months for the first three years and annually thereafter. Hierarchical clustering was used to divide the patients according to their baseline GI symptoms and manifestations. These were dysphagia, gastroesophageal reflux disease (GERD), peptic ulcer, bloating, constipation, diarrhea, malabsorption, and pseudo-obstruction. The characteristics and the disease outcomes of the clusters were compared.
Results: A total of 450 patients were included, with a mean follow-up of 5.3 years. Three symptom-based gastrointestinal (GI) clusters were identified: Cluster 1 (upper GI predominant), Cluster 2 (lower GI predominant), and Cluster 3 (diffuse GI involvement). GERD was highly prevalent across all clusters. The majority of patients (n = 406) belonged to Cluster 1, which was characterized by dysphagia (41%) and peptic ulcer disease (5%). Cluster 2 included 30 patients and was marked by bloating, constipation, and diarrhea. Cluster 3, the most severe phenotype, comprised 14 patients, all of whom had malabsorption; 93% had diarrhea, and 86% had dysphagia. Extraintestinal features also varied between clusters. Cluster 3 had the highest proportion of male patients (43%, P = 0.026) and diffuse cutaneous disease (91%, P = 0.037). Baseline forced vital capacity (FVC%) and modified Rodnan skin score (mRSS) did not differ significantly among the three groups. Although cluster 3 had higher mortality, it did not reach significance (P = 0.088).
Conclusion: Patients with systemic sclerosis exhibit distinct patterns of gastrointestinal symptoms at baseline. Recognizing these symptom-based clusters may improve risk stratification, help predict clinical outcomes, and inform clinical trial design for GI disease in patients with SSc.
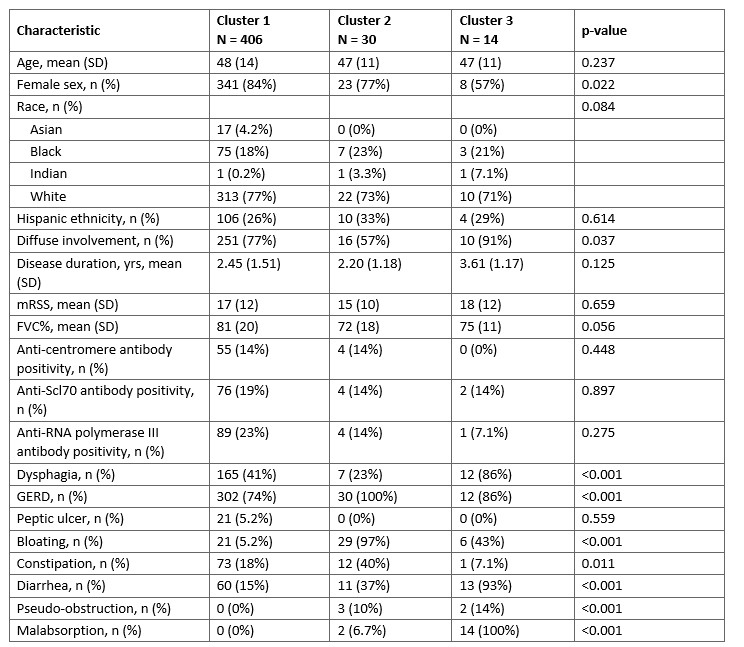 Table 1. Characteristics of Patients with Systemic Sclerosis Stratified by GI Symptom-Based Clusters
Table 1. Characteristics of Patients with Systemic Sclerosis Stratified by GI Symptom-Based Clusters
.jpg) Figure 1. Survival According to the Clusters
Figure 1. Survival According to the Clusters
To cite this abstract in AMA style:
Ayla A, Calderon Martinez E, Zhang M, Pedroza C, Chen B, Balar A, Hughes M, Bellando Randone S, Skaug B, Mayes M, Assassi S, McMahan Z. Symptom-Based Clustering of Gastrointestinal Involvement in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/symptom-based-clustering-of-gastrointestinal-involvement-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/symptom-based-clustering-of-gastrointestinal-involvement-in-systemic-sclerosis/
