Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: New therapies have improved the therapeutic management of juvenile idiopathic arthritis (JIA), allowing disease control in cases that are refractory or intolerant to methotrexate. However, satisfactory disease control is not achieved in all patients with the first biological and targeted synthetic therapies (ts/bDMARDs) and need switching to another. The choice of ts/bDMARDs for switching is made on an individual basis and influenced by several reasons, mainly the indication for each JIA category, but also previous drug discontinuation causes, concomitant therapy, and comorbidities. Therefore, clinicians are increasingly familiar with the clinical profiles of this treatments and the evidence in halting disease progression. In this study, we aimed to obtain information from real clinical practice about the management of JIA patients to characterize the trends in biologic utilization and switching among JIA categories.
Methods: We conducted a multicentre, observational, longitudinal study of JIA patients, following International League of Associations for Rheumatology (ILAR) classification categories: a) oligoarthritis; b) rheumatoid factor (RF) positive polyarthritis; c) RF negative polyarthritis; d) systemic arthritis; e) psoriatic arthritis; f) enthesitis-related arthritis. Our outcome measure was ‘switch’ (defined as ≥ 2 ts/bDMARDs courses for therapy). The independent variable was exposure to ts/bDMARDs including: a) TNF inhibitors (infliximab, adalimumab, etanercept, certolizumab, golimumab); b) Other bDMADRs: anti-IL6 (tocilizumab); anti-CTLA4 (abatacept); anti-IL1 (anakinra, canakinumab); anti-IL17 (secukinumab); anti-IL12/23 (ustekinumab); anti-CD20 (rituximab) c) tsDMARDs (tofacitinib). We did a descriptive analysis of the switching, stratified by JIA categories. We also did a bivariate analysis of variables associated with “difficult-to-treat” JIA (≥2ts/bDMARDs with different mechanisms of action)
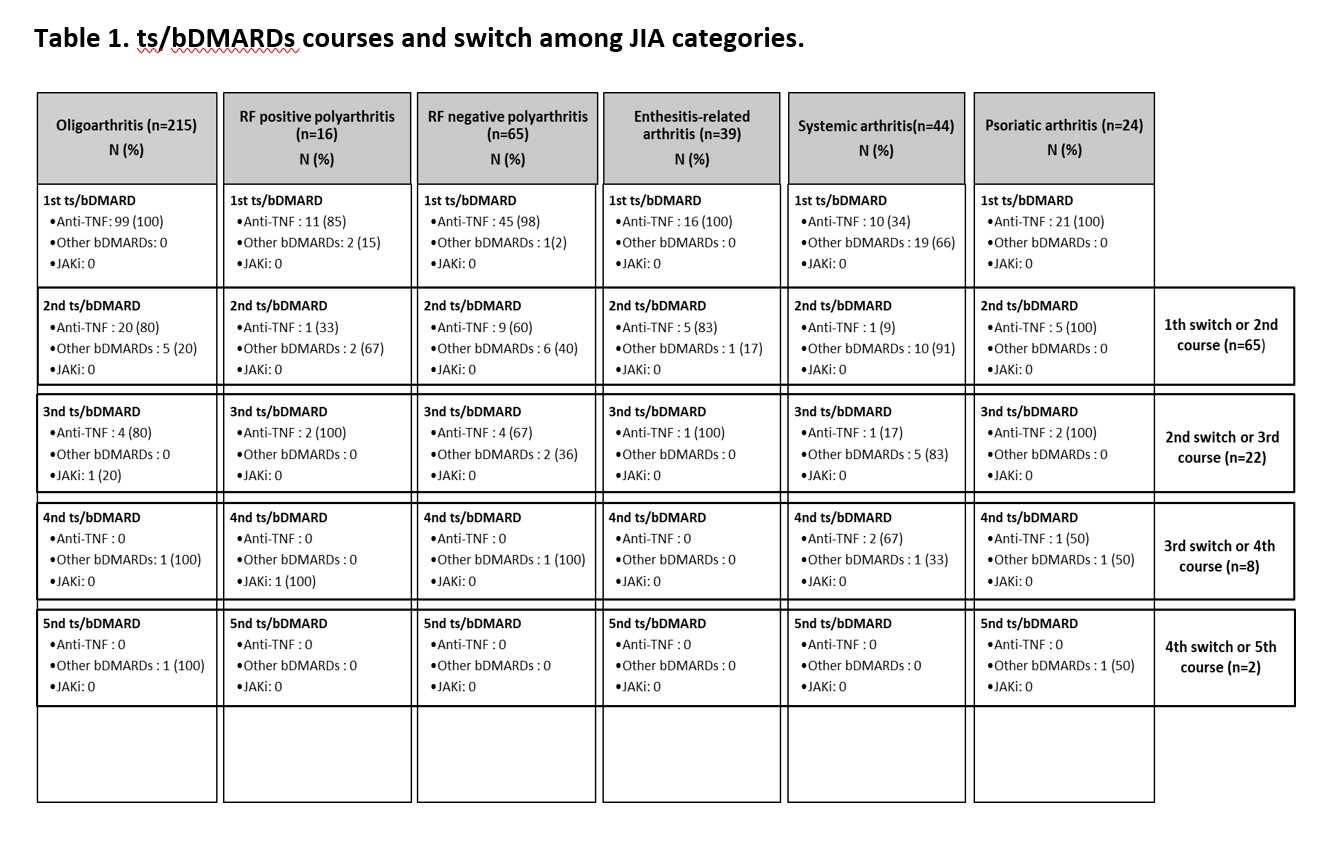
Results: In our cohort of 403 patients with JIA, the mean age at onset was 5.80 ± 4.46 years and 65.84% were females. A total of 235 (58.17%) patients received a bDMARD, with a total of 321 courses. Globally, TNF inhibitors were the most used bDMARDs, with 260 (81%) courses of treatment, although in systemic JIA, as expected, anti-IL1 and anti-IL6 were most used (Table 1). 28% of patients switched bDMARDs and we found a total of 97 ts/bDMARD switches. Of these, 28 (7%) patients met the definition of difficult-to-treat JIA patients. Our analysis identified that systemic JIA was the category with more changes among mechanisms of actions of ts/BDMARDs (p=0.001), representing 39% of the total switches. Long-term disease was also associated with high switching between ts/bDMARDs (p=0.01). Stratified analysis revealed distinct switching patterns in the different JIA categories (Table 1).
Conclusion: In this cohort, approximately a quarter of patients did not respond to the initial ts/bDMARD and need switching to another ts/bDMARD. Our stratified analysis found that the JIA category defines the choice of ts/bDMARD and treatment sequences. This real-world data study can give useful information about treatment patterns and trend for switching in routine clinical practice.
To cite this abstract in AMA style:
clemente Garulo D, Boteanu A, Trives Folguera L, García Fernández A, Abasolo l, Leon L, López Robledillo J, Nieto-Gonzalez J. Switching Patterns of Biological and Targeted Synthetic Therapies in Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/switching-patterns-of-biological-and-targeted-synthetic-therapies-in-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/switching-patterns-of-biological-and-targeted-synthetic-therapies-in-juvenile-idiopathic-arthritis/