Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Subglottic stenosis (SGS) is a recognized manifestation of granulomatosis with polyangiitis (GPA), occurring in 8–23% of patients. A distinct variant, identified in this study, involves edema of the inferior true vocal folds, termed “subcordal stenosis.” This pattern results in significant narrowing at a higher airway level than typical SGS, often extending inferiorly to involve the conventional subglottic region. Based on clinical observations, this pattern appears particularly responsive to glucocorticoid therapy. The objective of this study was to characterize the clinical presentation and treatment outcomes of subcordal stenosis and compare it to typical SGS associated with GPA. We hypothesized that patients with subcordal disease would require fewer dilations within two years of SGS diagnosis due to its glucocorticoid responsiveness.
Methods: Following IRB approval, we reviewed records of patients treated for SGS at the Johns Hopkins Vasculitis Center, identifying two groups: patients with subcordal involvement and those with typical SGS. Patients were excluded if they were procedurally treated for SGS before being seen at our institution. Subcordal cases were identified by searching laryngoscopy reports for “subcordal” and confirmed by otolaryngologist review as narrowing at the inferior true vocal folds (Figure 1). Baseline demographic and clinical characteristics were obtained through chart review. Longitudinal data on immunosuppressive treatments (start and stop dates) and tracheal dilation procedures were also collected. The number of tracheal dilations at two years was compared between groups using the Wilcoxon rank-sum test. Time-to-event analyses were performed, and Kaplan-Meier curves were compared using the log-rank test. All statistical analyses were conducted using R.
Results: Baseline characteristics of SGS patients with and without subcordal involvement are summarized in Table 1. Most patients in both groups had GPA diagnosed by rheumatologists. Five patients with subcordal disease also had typical subglottic involvement, while six had isolated subcordal disease. Among patients with subcordal involvement, 10 of 11 received prednisone at the time of SGS diagnosis. Patients with subcordal disease underwent fewer dilations within two years compared to those without subcordal involvement (median 0 vs. 1 dilation, p = 0.05, Table 1). Kaplan-Meier analysis showed that patients with subcordal involvement had a significantly longer time to first dilation, with a median of 792 days compared to 44 days in those without subcordal disease (p = 0.048, Figure 2).
Conclusion: Among patients with SGS seen at our vasculitis center (most of whom have GPA), those with subcordal involvement exhibit a reduced need for tracheal dilation and a longer interval before first dilation compared to patients without subcordal disease. These findings likely reflect greater corticosteroid responsiveness in patients with subcordal airway involvement.
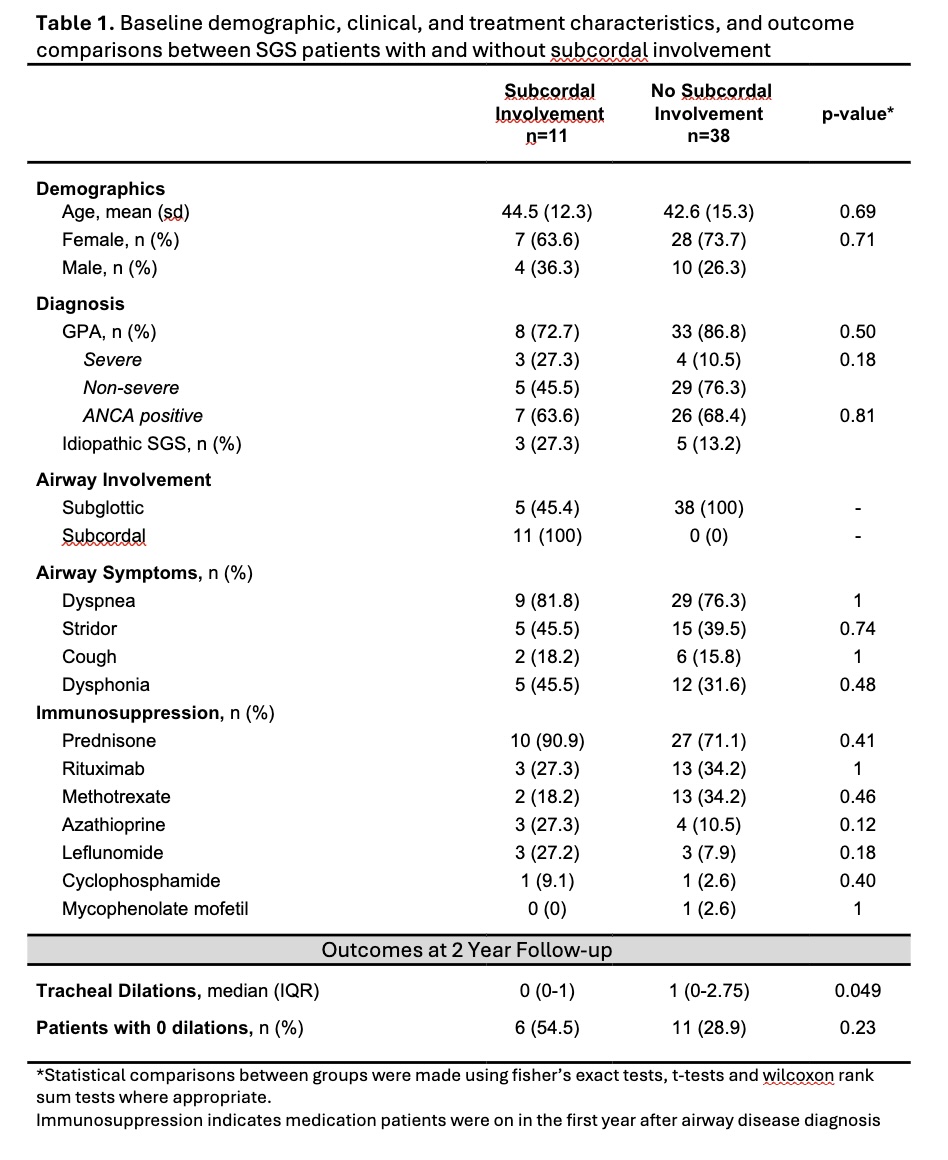 Table 1. Baseline demographic, clinical, and treatment characteristics, and outcome comparisons between SGS patients with and without subcordal involvement
Table 1. Baseline demographic, clinical, and treatment characteristics, and outcome comparisons between SGS patients with and without subcordal involvement
.jpg) Figure 1. Representative laryngoscopic images of subglottic stenosis with and without subcordal involvement and animated depiction of subcordal stenosis.
Figure 1. Representative laryngoscopic images of subglottic stenosis with and without subcordal involvement and animated depiction of subcordal stenosis.
.jpg) Figure 2. Kaplan-Meier curves for time to first tracheal dilation in patients with subcordal stenosis versus subglottic stenosis.
Figure 2. Kaplan-Meier curves for time to first tracheal dilation in patients with subcordal stenosis versus subglottic stenosis.
To cite this abstract in AMA style:
Denvir B, Antiochos B, Seo P, Hillel A. Subcordal Stenosis is a Glucocorticoid-Responsive Manifestation of Granulomatosis with Polyangiitis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/subcordal-stenosis-is-a-glucocorticoid-responsive-manifestation-of-granulomatosis-with-polyangiitis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subcordal-stenosis-is-a-glucocorticoid-responsive-manifestation-of-granulomatosis-with-polyangiitis/
