Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular (CV) mortality and morbidity is increased in ankylosing spondylitits (AS) as compared to the general population. Carotid plaque, considered as a surrogate marker for atherosclerosis associated with very high CV risk, is more prevalent in AS patients than in healthy controls. Nevertherless, we have no consistent data about subclinical atherosclerosis (SA) in non-radiographic axial spondyloarthritis (nr-axSpA). In this study we assessed the SA in nr-axspA compared with AS in the largest series studied so far, and established a predictive model to identify patients with high CV risk.
Methods: This is a transversal observational study from the AtheSpAin cohort, a Spanish multicenter cohort to study atherosclerosis in axSpA. We compared patients with AS vs those with nr-axSpA according to ASAS criteria. Carotid ultrasound (US) examination was done in all patients, included the measurement of carotid intima-media wall thickness (cIMT) in the common carotid artery and the detection of plaques in the extracranial carotid tree bilaterally, according to the Mannhein consensus. CV risk was calculated according to the systematic coronary risk evaluation (SCORE).
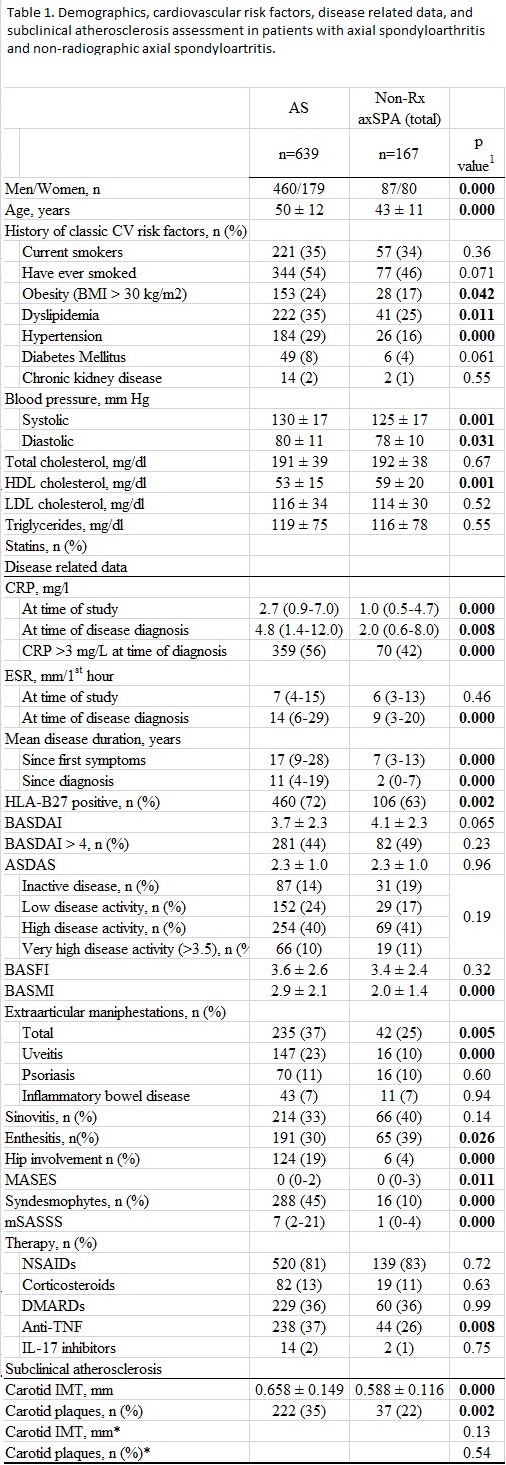
Results: A set of 639 patients with AS and 167 patients with nr-axSpA were recruited in this study. Patients with AS were mainly men, older and had a higher prevalence of cardiovascular risk factors compared to nr-axSpA patients. They also had higher levels of C reactive protein and estimated (CPR) and erythrocyte sedimentation rate (ESR). Comparison of baseline characteristics and clinical features between patients with AS and nr-axSpA is shown in table 1. After adjusting data for age, sex and cardiovascular morbidity, no difference in the prevalence of carotid plaques or in the carotid IMT was found between both groups.
We then analyzed the prevalence of carotid plaques in the groups of low and moderate CV risk according to the SCORE, finding no differences between AS and nr-axSpA (10.7 % Vs 10.1%, p=0.9 and 40.5 % Vs 45.5 %,p=0.94 respectively)
Considering the comparable atherosclerotic burden observed in nr-axSpA and AS, we designed a model to identify those patients diagnosed with any of these conditions with very high CV risk because of the presence of carotid plaques. A predictive model which included SCORE plus age, BASFI and ESR at time of disease diagnosis in patients with moderate SCORE showed a high specifity (88%) to detect very high risk patients, but with a limited sensitivity (41%) table 2. The AUC of this model was found to have higher discrimination than the SCORE AUC ( 0.652 Vs 0.592, p= 0,025).
Conclusion: SA disease in patients with nr-axSp is similar to those with AS, despite the higher inflammatory state of the latter. Many patients with axSpA with a moderate risk of CV events according to the SCORE are reclassified into very high risk after carotid US examination. Patients with higher age, ESR at the diagnosis of axSpA and BASFI are more likely to present carotid plaques in US examination.
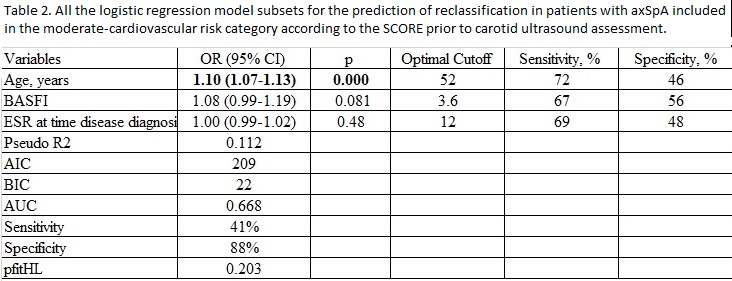 Values in bold face are statistically significant. AIC: Akaike information criterion; BIC: Schwarz Bayesian criterion AUC: area under the curve; pfitHL: Hosmer-Lemeshow goodness-of-fit DMARD: disease-modifying antirheumatic drug; BASMI Bath Ankylosing Spondylitis Metrology Index.
Values in bold face are statistically significant. AIC: Akaike information criterion; BIC: Schwarz Bayesian criterion AUC: area under the curve; pfitHL: Hosmer-Lemeshow goodness-of-fit DMARD: disease-modifying antirheumatic drug; BASMI Bath Ankylosing Spondylitis Metrology Index.
To cite this abstract in AMA style:
Gonzalez-Mazon I, Rueda-Gotor J, Ferraz-Amaro I, Sanchez-Bilbao L, Martinez-Lopez D, Genre F, Palmou Fontana N, Calvo-Río V, Remuzgo-Martínez S, Pulito-Cueto V, Corrales A, Lera-Gómez L, Portilla V, Mata C, Hernández-Hernández V, Castañeda S, Vicente-Rabaneda E, Fernandez-Carballido C, Martínez-Vidal M, Castro-Corredor D, Anino-Fernández J, Quevedo-Abeledo J, Rodríguez-Lozano C, García Vivar, M, Galínez-Agirregoikoa E, Fernandez-Diaz C, Llorca J, López-Mejías R, Montes-Perez E, Peiteado D, Plasencia C, Balsa-Criado A, Barbarroja N, Ladehesa-Pineda L, Ortega-Castro R, Collantes-Estévez E, Blanco R, González-Gay M. Subclinical atherosclertoic disease in ankylosing spondylitis and non-radiographic axial spondyloarthritis. A multicenter study with 806 patients. [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/subclinical-atherosclertoic-disease-in-ankylosing-spondylitis-and-non-radiographic-axial-spondyloarthritis-a-multicenter-study-with-806-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subclinical-atherosclertoic-disease-in-ankylosing-spondylitis-and-non-radiographic-axial-spondyloarthritis-a-multicenter-study-with-806-patients/