Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose
A prediction rule for knee osteoarthritis (OA) progression would have great clinical utility in identifying at-risk patients for intervention. Rules using clinically available measurements have so far demonstrated modest predictive ability. Dual energy X-ray absorptiometry is widely available and provides rapidly evaluable quantitative data on tibial subchondral bone mineral density (BMD) that is associated with OA severity.
Our goal was to create a prediction rule for medial joint space loss (a proxy for OA progression) based on clinical factors; and to quantify the benefit of adding the ratio of the periarticular medial to lateral bone mineral density (M:L paBMD) to the rule.
Methods
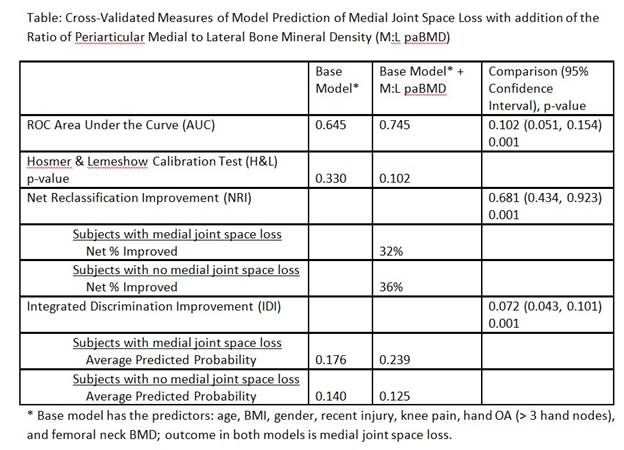
Subjects were from the Osteoarthritis Initiative (OAI) progression subcohort, with X-ray readings at both 24- and 48-month visits, medial joint space score < 3 at 24 months, and a valid 30- or 36-month BMD value. Weight-bearing PA fixed flexion knee X-rays were assessed for medial tibio-femoral joint space using the OARSI atlas. Knees were imaged with GE Lunar Prodigy Advance scanners, providing M:L paBMD values. Loss of medial joint space, including within OARSI grade worsening, between 24 and 48 months was used as the outcome in logistic regression for the prediction models. Clinical factors chosen for their predictive ability from 24 months were considered for the base model. M:L paBMD was added to the base model to determine if it materially improved prediction, with cross-validation used in this evaluation. Discriminative ability was based on the area under the ROC curve (AUC) and calibration by the Hosmer & Lemeshow test (H&L). The benefit of adding M:L paBMD was evaluated by 1) change in AUC, 2) net reclassification improvement (NRI) based on the percent of subjects with improved prediction, and 3) integrated discrimination improvement (IDI) based on the mean improvement in predicted probabilities.
Results
496 subjects were included; 68 (14%) experienced medial joint space loss; 48% were female; 15%, 16%, 36%, 30%, and 3% respectively had Kellgren & Lawrence scores 0 – 4; 2% had recent knee injury; 35% had hand OA (> 3 nodes) on physical exam at OAI entry. The mean (SD) for age was 64.4 (9.2) years; BMI 29.5 (4.9) kg/m2; VAS knee-specific pain 3.4 (2.9) on a 0-10 scale; femoral neck BMD .96 (.15) g/cm2; and M:L paBMD 1.1 (.14). The base model included age, BMI, gender, recent injury, knee pain, hand OA, and femoral neck BMD as predictors. The change in AUC, NRI and IDI were statistically significantly improved in the model with M:L paBMD (Table). The H&L test did not find poor calibration in either model.
Conclusion
The M:L BMD ratio provided a meaningful improvement in predictive ability for 2-year medial joint space loss compared to using only clinical predictors. An instrument combining clinical characteristics with M:L paBMD may be useful as a predictive tool for structural progression in patients with knee OA.
Disclosure:
M. P. Lavalley,
None;
G. H. Lo,
NIH/NIAMS,
2;
L. L. Price,
NIAMS-NIH,
2;
J. Driban,
None;
C. Eaton,
None;
T. E. McAlindon,
NIAMS-NIH,
2.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subchondral-bone-mineral-density-improves-prediction-of-knee-osteoarthritis-progression-compared-with-clinical-factors-alone-data-from-the-osteoarthritis-initiative/