Session Information
Date: Sunday, November 12, 2023
Title: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Ischemic stroke is 2-3 times more common in patients with SLE as compared to the general population, and genetic susceptibility in the STAT4 and HLA-DRB1 genes have been reported to contribute to stroke in SLE. But few studies have investigated the distribution of stroke sub-types in SLE, and to our knowledge, none if they are associated with known susceptibility genes. We therefore investigated the distribution of ischemic stroke sub-types, classified according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) system(1), among patients with systemic lupus erythematosus (SLE).
Methods: Among 665 SLE patients fulfilling ACR -97 criteria for SLE, we identified 69 patients with ischemic stroke. Medical charts were retrieved and brain, cardiac and vascular imaging at the time of the first stroke were examined. Classification was performed according to TOAST: large-artery atherosclerosis (LAA), cardioembolism (CE), small-artery occlusion (SAO), stroke of other determined etiology (OC) and stroke of undetermined etiology (UE). Occurrence of the anti-phospholipid syndrome/antibodies (APS/aPL) were documented. Evaluators were blinded to genotypes. General population controls (N=658) and SLE patients free from previous cerebrovascular disease (N= 517) were used as comparators. Genetic susceptibility in the signal transducer and activator of transcription factor 4 (STAT4) gene, defined by the single nucleotide polymorphism (SNP) rs10181656(G), and the Human Leukocyte antigen (HLA)-DRB1 alleles were explored.
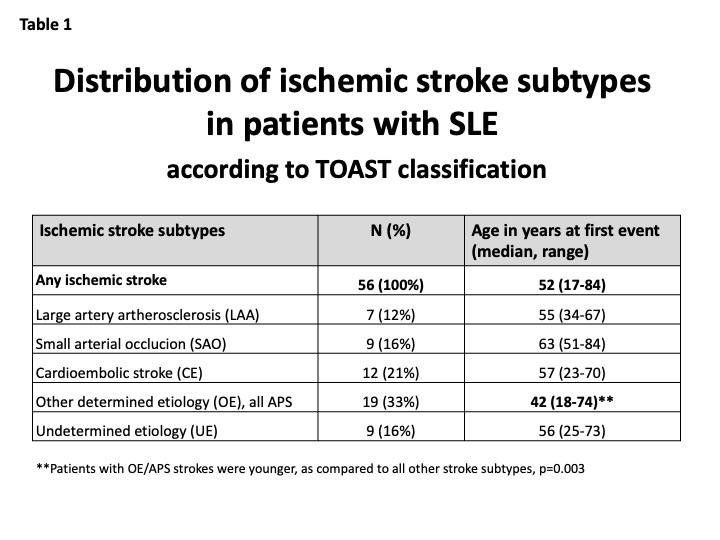
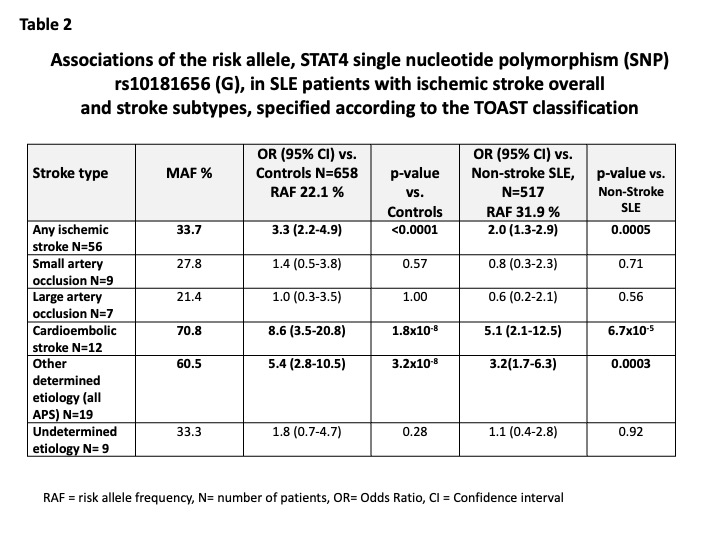
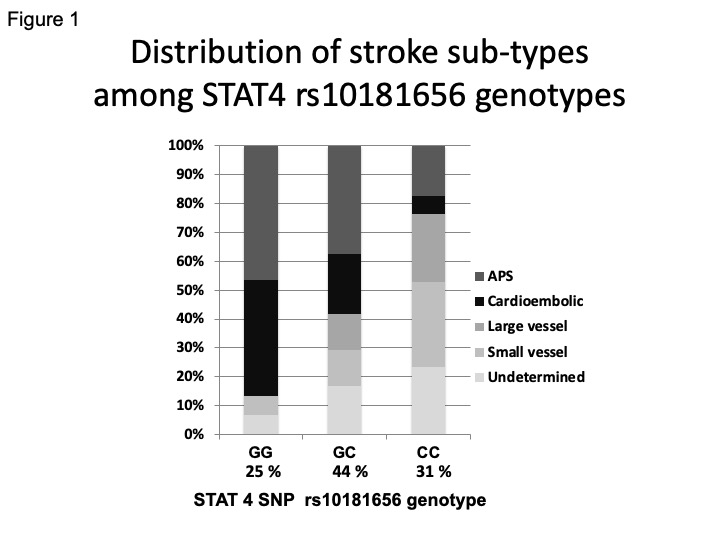
Results: 56/69 patients with ischemic stroke had charts with sufficient information for TOAST classification. Median age was 52 (17-84) years, 91% were female. TOAST classification and age at first stroke is presented in Table 1. All strokes classified as OC were attributed to APS/aPL. Strokes of OE/APS and CE origin were associated with the STAT4 risk genotype as presented in Table 2 and Figure 1. HLA-DRB1 alleles were not associated with stroke sub-types (data not shown).
Conclusion: The majority (54%) of ischemic strokes among 56 SLE patients were of APS/aPL or CE origin. These two subtypes were associated with genetic susceptibility in the STAT4 gene. We also noted that patients with APS/aPL associated strokes were younger than other sub-types, median 42 years. STAT4 genotype could, in addition to antiphospholipid antibodies and echocardiography, add information about stroke risk and help identify patients who will benefit from prophylactic anticoagulation treatment.
To cite this abstract in AMA style:
Hopia L, Laveskog A, Leonard D, Jonsen A, Gustafsson J, Gunnarsson I, Zickert A, Nordmark G, Bengtsson A, Padyukov L, Sandling J, Syvänen A, Rönnblom L, Andersson M, Svenungsson E. Sub-types of Ischemic Stroke in Systemic Lupus Erythematosus,-associations with STAT4 and HLA-DRB1 Risk Genotypes [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/sub-types-of-ischemic-stroke-in-systemic-lupus-erythematosus-associations-with-stat4-and-hla-drb1-risk-genotypes/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sub-types-of-ischemic-stroke-in-systemic-lupus-erythematosus-associations-with-stat4-and-hla-drb1-risk-genotypes/