Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The Centers for Disease Control and Prevention director has said “nothing will save more lives” than protocols to control blood pressure (BP). BP is relevant in rheumatology clinics because it is causally linked to cardiovascular disease. Hypertension control is also one of ten RA quality measures endorsed by ACR and Medicare for 2017 quality payment reporting. Yet, minimal evidence exists on how to improve BP control in busy rheumatology clinics. We previously implemented a staff protocol that doubled timely follow-up after high BPs in rheumatology clinics, and now aimed to examine its impact on population BP control.
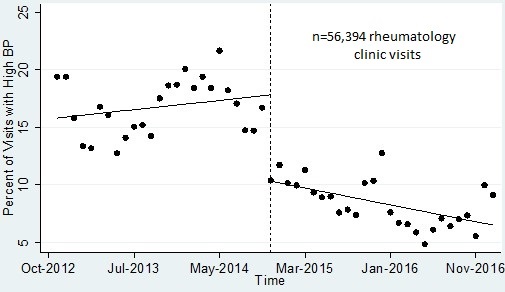
Methods: We assessed population trends in the rate of monthly high BPs (% of all visits) before and after the implementation of a staff BP Connect Health protocol in three rheumatology clinics (10/2012-10/2014 vs. 11/2014-12/2016). During implementation, clinical educators trained nurses and medical assistants in an hour-long session on BP in rheumatic diseases, proper BP measurement, and the BP Connect Health protocol steps. Protocols included EHR prompts to re-measure high BPs, and if confirmed high, offer timely primary care follow-up. Follow-up orders automatically routed to scheduling staff for patients with in-network primary care, and printed on after visit materials for all patients. EHR data reported the monthly percentage of adult rheumatology clinic visits with an initial BP >140/90 mmHg.
We performed time series regression with Newey-West standard errors to examine changes in rates of high BPs in the 24 months before and after protocol implementation.
Results: A total of 28,109 pre-protocol rheumatology clinic visits were compared to 28,285 visits after protocol implementation. Monthly rates of high BP, when averaged over the periods before and after implementation, fell from 17% pre- to 8% post-protocol. Time series analysis demonstrated a significant reduction after protocol implementation and continued improvement over time (Figure 1. p<0.003 & p<0.03). Strengths included 2-year protocol feasibility; limitations include our single center pre-post design.
Conclusion: After implementing the rheumatology staff protocol, we observed a 9% reduction in mean rates of high BP across rheumatology clinic populations. Early improvements likely reflected staff BP training, while later improvements may reflect improved follow-up, adherence, and management of BP. Future multi-site studies will test the BP Connect Health protocol in other rheumatology and specialty populations at risk for cardiovascular disease.
To cite this abstract in AMA style:
Bartels CM, Ramly E, Sampene E, Lauver D, McBride P, Johnson H. Staff Protocol in Rheumatology Clinics Reduces Population-Level Rate of High Blood Pressure [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/staff-protocol-in-rheumatology-clinics-reduces-population-level-rate-of-high-blood-pressure/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/staff-protocol-in-rheumatology-clinics-reduces-population-level-rate-of-high-blood-pressure/