Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Based on data from the Osteoarthritis Initiative (OAI), MRI-based analyses of bone shape changes in the knee predict symptomatic and radiographic progression of knee OA and risk of joint replacement (Neogi 2013; Barr 2016). In a 12-month, double-blind, placebo-controlled trial of MRI-confirmed bilateral patellofemoral OA, TPX-100, administered in 4 weekly injections (200 mg/injection), markedly improved knee physical function (KOOS/WOMAC) compared with identical placebo injections (McGuire 2017). At 12 months, there were no significant treatment differences in overall knee pain; however, pain frequency significantly decreased in TPX-100-treated knees compared with placebo-exposed knees, and overall analgesic use declined by >60%. In the current retrospective study, we investigated patellar bone-shape change from baseline to 12-months among subjects who participated in TPX-100-1 and analyzed the strength of association between patellar bone shape change and changes in knee pain frequency.
Methods: Patellar bone shape changes from baseline were analyzed centrally by an automated method (Imorphics, Inc.) blind to treatment assignment and clinical results. MRI image quality permitted analysis in 79 of 93 subjects (85%) using active appearance model (AAM). Bone shape scores were computed to discriminate normal (non-OA) shapes versus bone surface deformations associated with radiographic and symptomatic OA. Changes in pain frequency were determined using Question 1 from the KOOS pain domain: “How often do you experience RIGHT/LEFT knee pain?” Spearman analysis was performed to investigate correlations between patellar shape change and change in knee pain frequency.
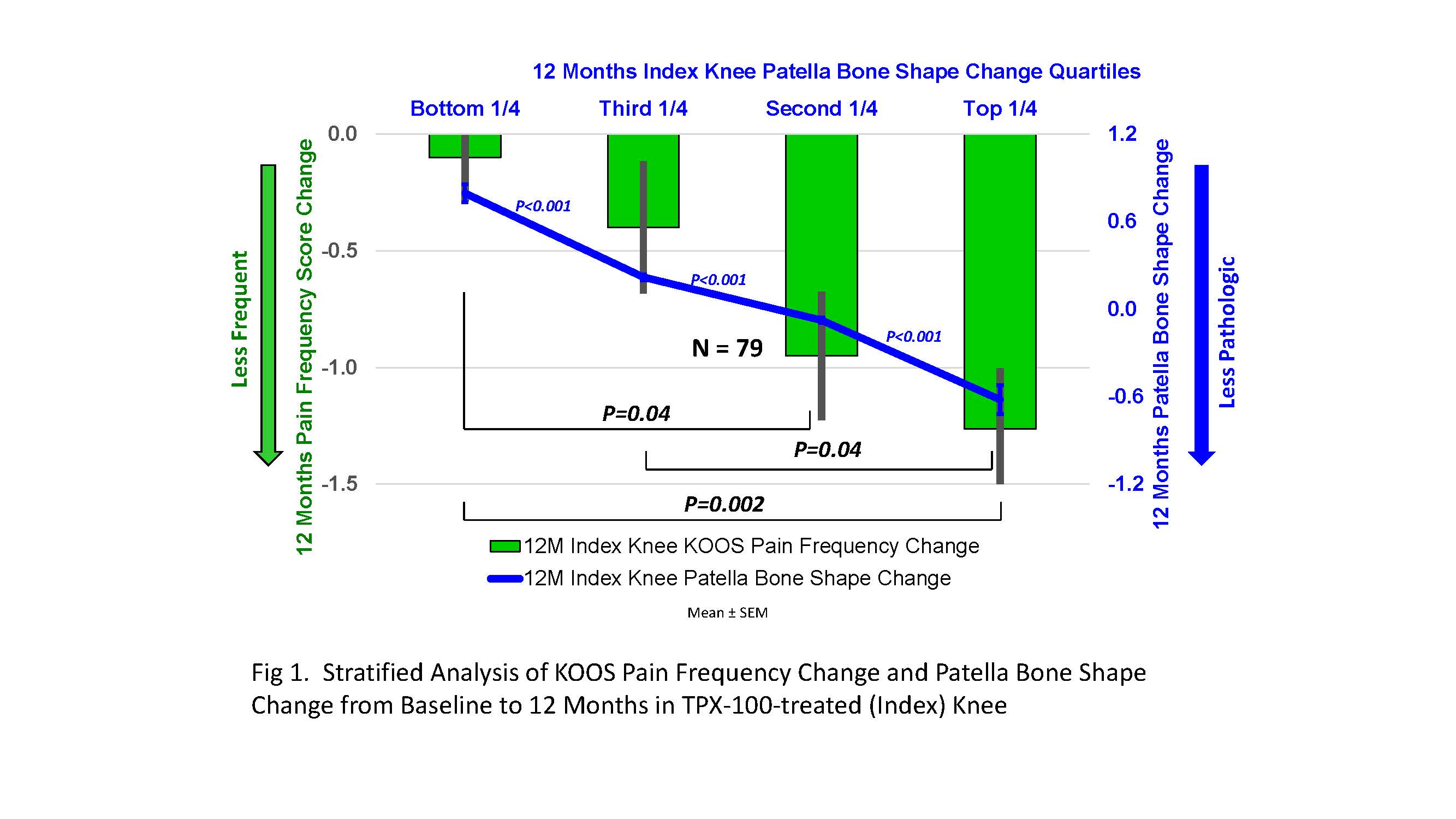
Results: Pain frequency was significantly improved in TPX-100-treated knees compared with placebo-exposed knees. Patellar bone shape delay correlated significantly with pain frequency reduction (r=.411; p=.0002; Table 1). Knees with stabilized or reduced bone-shape changes at 12 months had the greatest reductions in pain frequency, with statistically significant differences between quartiles (Fig 1).
Conclusion: In subjects with MRI-confirmed bilateral PFOA, a single series of IA TPX-100 is associated with statistically significant and clinically meaningful reductions in knee pain frequency at 12 months, significantly correlated with reduced or stabilized pathologic patellar bone shape change compared with placebo. Quartile analysis suggests a “dose-response” relationship between reduced patellar bone shape change and reduced knee pain frequency in TPX-100-treated knees. These concordant structural and symptomatic benefits support development of TPX-100 as a candidate DMOAD as well as further study of bone shape change as an imaging biomarker in knee OA.
References
Neogi T, et. al. Arthritis Rheum. 2013;65(8):2048–2058
Barr AJ, et. al. Rheumatology (Oxford). 2016;55(9):1585–1593
ACR 2019 Patella Bone shape vs Pain Figure 1
To cite this abstract in AMA style:
McGuire D, Bowes M, Brett A, Segal N, Miller M, Rosen D, Kumagai Y. Stabilization of Patellar Bone-Shape Correlates Significantly with Reduced Knee Pain Frequency After IA TPX-100 in Subjects with Bilateral Patellofemoral OA [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/stabilization-of-patellar-bone-shape-correlates-significantly-with-reduced-knee-pain-frequency-after-ia-tpx-100-in-subjects-with-bilateral-patellofemoral-oa/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/stabilization-of-patellar-bone-shape-correlates-significantly-with-reduced-knee-pain-frequency-after-ia-tpx-100-in-subjects-with-bilateral-patellofemoral-oa/

