Session Information
Date: Saturday, November 12, 2022
Title: Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: It has been reported that 20-50% of patients with PMR have subclinical GCA. The natural history of US-defined subclinical GCA in PMR is not known.
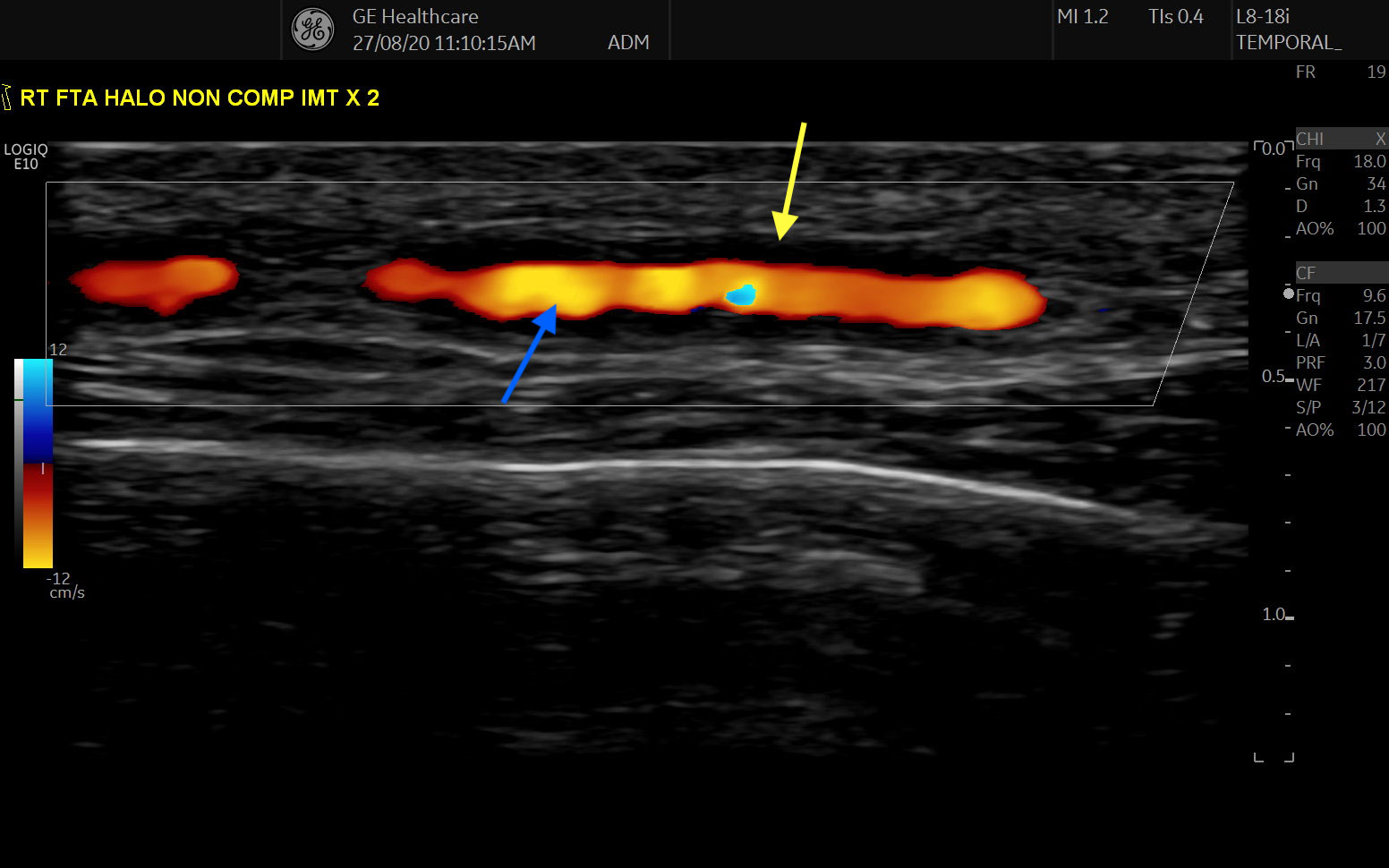
Methods: Twenty five newly-diagnosed PMR patients who met a clinical diagnosis for PMR, verified by 2 rheumatologists, were examined by US. US of all 6 branches of the superficial temporal arteries and both axillary arteries was performed using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign (Fig. 1) and non-compressible arteries with a thickened intima-media complex. In the axillary arteries, a halo sign and an intima-media thickness of >1.0mm was considered positive. Follow-up consultations after 1 year were undertaken to review the clinical diagnosis. In our subclinical GCA group, a PMR-dose steroid taper was used in those with a prompt clinical response, a GCA-dose steroid taper was initiated for those who subsequently flared and Tocilizumab was initiated in the event of a second flare.
Results: Our cohort consisted of 64% females (n=16) with a mean age of 67 years (range 50-84). 2012 ACR/EULAR classification criteria were met in 16/25 patients (primarily due to prior corticosteroid use in primary care resulting in normal ESR/CRP).
Five patients (20%) were identified as having subclinical GCA on US (5/5 met 2012 ACR/EULAR PMR classification criteria, 0/5 met ACR GCA classification criteria). Temporal artery involvement was identified in 5/5, with axillary involvement in 1/5. Mean halo count was 3 (range 1-5) and mean halo score was 21.2 (range 17-29).Two patients were managed with an initial PMR-dose of prednisolone but relapsed. Three patients were treated with an initial GCA-dose of steroids, all of whom relapsed.
At a median of 12 months follow up 1/20 (5%) of the PMR-only cohort had developed clinical signs of GCA. 5/5 (100%) of the subclinical GCA cohort had developed a clinical diagnosis of GCA with 3/5 requiring an increase in steroid dose and 2/5 requiring Tocilizumab. At 12 months follow up 0% of patients had developed ischaemic complications.
Conclusion: Our study indicates that a single screening US of temporal and axillary arteries accurately identified 83.3% of patients with subclinical GCA in an inception PMR cohort. Our experience indicates that these patients are likely to be resistant to PMR-dose steroids and ultimately may require biologic therapy.
To cite this abstract in AMA style:
Kirby C, Flood R, Mullan R, Murphy G, Kane D. Sonographic Prevalence of Subclinical GCA in Newly Diagnosed PMR [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/sonographic-prevalence-of-subclinical-gca-in-newly-diagnosed-pmr/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sonographic-prevalence-of-subclinical-gca-in-newly-diagnosed-pmr/