Session Information
Date: Sunday, November 5, 2017
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment Poster I: Biomarkers and Outcomes
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
The urokinase plasminogen activator receptor (uPAR) is expressed on various cell types and plays important roles in proteolysis, migration and adhesion. Receptor shedding yields a soluble form (suPAR) that has emerged as a promising severity biomarker in malignancies, inflammatory and infectious diseases. Previously, suPAR was shown to reflect accumulated organ damage in systemic lupus erythematosus (SLE). Our aim was to investigate suPAR as a potential predictor of future organ damage in well-characterized patients with recent-onset SLE.
Methods:
A total of 345 patients with SLE (≥4 ACR criteria) were included in this study. All patients originated from the SLICC inception cohort and were selected based on a minimum of 5-years follow-up and absence of organ damage (SLICC/ACR damage index; SDI>0) at inclusion. The patients were enrolled within 15 months of SLE diagnosis. Plasma creatinine was available for 180 patients and estimated glomerular filtration rate (eGFR) was calculated according to the MDRD 4-Variable Equation. Serum suPAR levels were measured by ELISA (Virogates, Birkerod, Denmark) at inclusion only, and levels at inclusion were related to SDI after 5-years of follow-up. Age- and sex-matched controls (1:1) were from the Swedish population.
Results:
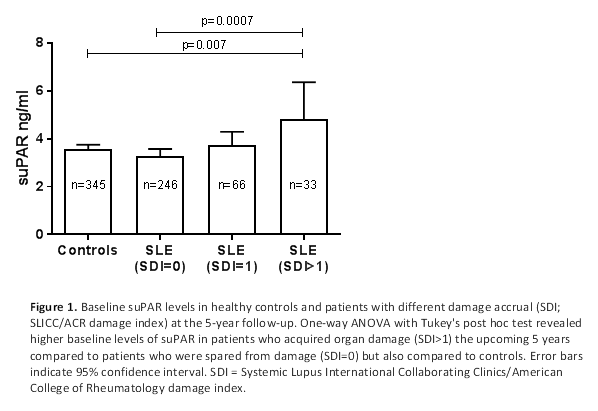
Baseline suPAR levels were higher in patients who acquired damage (SDI >1) over a 5-year period (n=33) compared to patients without damage development (n=246; p<0.001) and controls (n=345; p=0.007) (Fig. 1). There were no significant differences in suPAR levels with regard to ethnicity (Caucasians vs. non-Caucasians) or sex in patients and controls, but there was a weak correlation between age and suPAR among controls (p<0.001, r=0.23). No correlations (r>0.2) were found between suPAR and disease activity (SLEDAI-2K), corticosteroid dose or eGFR in patients. Logistic regression revealed significant impact of baseline suPAR on future damage (SDI>1) (p=0.014; area under curve, AUC=0.64) and the predictive value became stronger after adjustment for age, sex, ethnicity and corticosteroid dose (p=0.008; AUC=0.74). Examining the components of the SDI individually revealed significant impact of suPAR on damage in the musculoskeletal domain (SDI≥1) (p=0.018; AUC=0.66) also when adjusting for covariates (p=0.020; AUC=0.68).
Conclusion:
Prognostic biomarkers of disease severity in SLE could identify patients in need of tight control and improved treatment strategies. suPAR has become an interesting option for patient triaging and prognostication in various diseases, and here, for the first time, it is shown to have predictive potential of damage accrual in SLE. Continued follow-up of patients could elucidate the association between suPAR and damage in specific organ domains. Furthermore, the possible role of suPAR as a causative agent in SLE organ damage remains to be investigated.
To cite this abstract in AMA style:
Enocsson H, Wirestam L, Wetterö J, Skogh T, Bruce IN, Sjöwall C. Soluble Urokinase Plasminogen Activator Receptor (suPAR) Predicts the Development of Organ Damage over 5 Years in Systemic Lupus Erythematosus: Results from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/soluble-urokinase-plasminogen-activator-receptor-supar-predicts-the-development-of-organ-damage-over-5-years-in-systemic-lupus-erythematosus-results-from-the-systemic-lupus-international-collaborat/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/soluble-urokinase-plasminogen-activator-receptor-supar-predicts-the-development-of-organ-damage-over-5-years-in-systemic-lupus-erythematosus-results-from-the-systemic-lupus-international-collaborat/