Session Information
Date: Tuesday, November 15, 2016
Title: Rheumatoid Arthritis – Small Molecules, Biologics and Gene Therapy - Poster III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is an autoimmune disease characterized by chronic inflammation of the synovial joints and infiltration by activated macrophages. TNFa is a central mediator in the process, leading to joint swelling and subsequent articular destruction. CD163 is a scavenger receptor expressed by M2C macrophages. We previously reported the soluble (s) form to be associated with disease activity and reflect discontinuation of anti-TNFa treatment in RA2. The mannose receptor, CD206, is also a scavenger receptor, but expressed by M2A-macrophages and dendritic cells. It is involved in collagen internalization and degradation. The soluble form is suggested as biomarker of M2A-macrophage activation. In this study, we investigate sCD206 plasma levels in early RA patients, before, during and after anti-TNF_ treatment.
Methods: Plasma levels of sCD206 was measured by ELISA in samples from 155 early RA patients belonging to the OPERA cohort[1]. Age 53.5 years 70% females, average disease duration: 3 months. Patients were randomized to 12 months conventional methotrexate and placebo (PLA) or methotrexate and adalimumab (ADA) treatment, followed by open-label treatment with DMARD and if needed adalimumab. The disease was assessed at baseline and after 3, 6, 12 and 24 months by: Disease Activity Score (DAS28), Health Assessment Questionnaire (HAQ), C-Reactive Protein (CRP), Swollen Joint Counts (SJC40), Tender Joint Counts (TJC40), Clinical Disease Activity Index (CDAI), Visual Analogue Scale (VAS) for pain, IgM-RF and anti-CCP. Statistical analysis was performed by studentÕs t-test, SpearmanÕs Rank correlation and linear regression.
Results: Baseline plasma level of sCD206 in treatment na•ve RA patients was 0.33 mg/l (CI: 0.33 mg/l Ð 0.38 mg/l) corresponding to the upper part of the reference interval for healthy controls (0.10 mg/l Ð 0.43 mg/l). Anti-TNFa treatment significantly decreased plasma sCD206, whereas discontinuation of anti-TNFa resulted in increasing sCD206 plasma levels. In the PLA group, sCD206 levels was decreased after 3 months, and did not differ from those at baseline after 6 months. In the ADA group, however, levels remained lower than baseline throughout the treatment period (Figure 1). Soluble CD206 correlated with previously measured sCD163[2] at all 5 time points (r2: 0.24-0.38, p<0.001). Soluble CD206 did not correlate with clinical nor biochemical disease markers, however sCD206 increased when adalimumab was discontinued.
Conclusion: Plasma sCD206 decreased with treatment in early RA patients. Treatment with anti-TNFa preserved this decrease in the entire follow-up period; however, discontinuation of anti-TNFa was reflected by increasing sCD206 plasma levels. Soluble CD206 did not reflect disease activity in early RA, but like sCD163, reflected anti-TNFa treatment. Figure 1 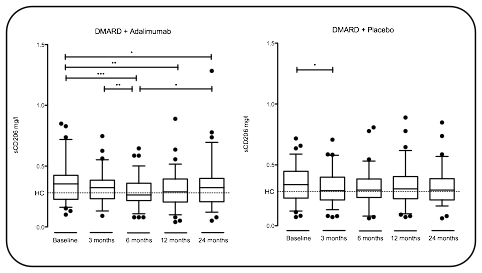
[1] Horslev-Petersen, K. et al. Ann Rheum Dis (2013)
[2] Greisen, S. R. et al. Clin Exp Rheumatol (2011)
To cite this abstract in AMA style:
Heftdal LD, Stengaard-Pedersen K, Lund Hetland M, Hørslev-Petersen K, Junker P, Østergaard M, Hvid M, Deleuran B, Møller HJ, Greisen S. Soluble CD206 Plasma Levels Decreases with Treatment and Reflects Anti-Tnfa Discontinuation in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/soluble-cd206-plasma-levels-decreases-with-treatment-and-reflects-anti-tnfa-discontinuation-in-rheumatoid-arthritis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/soluble-cd206-plasma-levels-decreases-with-treatment-and-reflects-anti-tnfa-discontinuation-in-rheumatoid-arthritis/
