Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Prior studies have shown that RA outcomes, including disease activity, erosions, and disability, are worse among patients with low socioeconomic status (SES). However, few studies have examined the relationship between RA functional outcomes and SES at the national level. We used the ACR’s Rheumatology Informatics System for Effectiveness (RISE) registry to investigate the relationship between individual SES and functional status (FS) among individuals with RA across U.S. rheumatology practices.
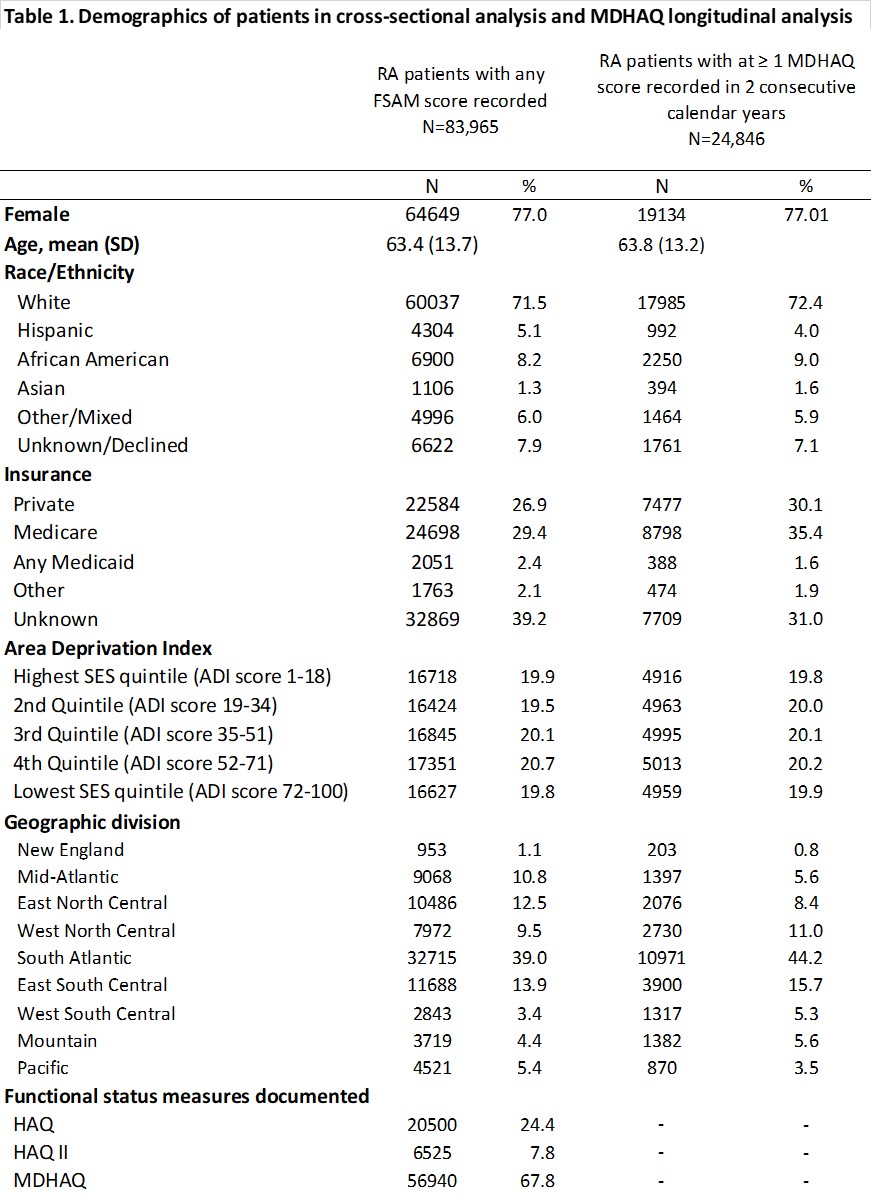
Methods: Data derived from RISE, a national EHR-enabled registry that passively collects data on all patients seen by participating rheumatology practices. As of 2018, RISE held validated data from 1,113 providers in 226 practices, representing about 32% of the U.S. clinical rheumatology workforce. Patients included in this study were ≥18 years old, had ≥ 2 visits with RA codes ≥ 30 days apart, and ≥ 1 FS measure (MDHAQ, HAQII, or HAQ) in 2016-2018. As a proxy for SES, we used the Area Deprivation Index (ADI) score, a 9-digit ZIP-code-based indicator of neighborhood socioeconomic disadvantage (range 1-100, higher score = lower SES).
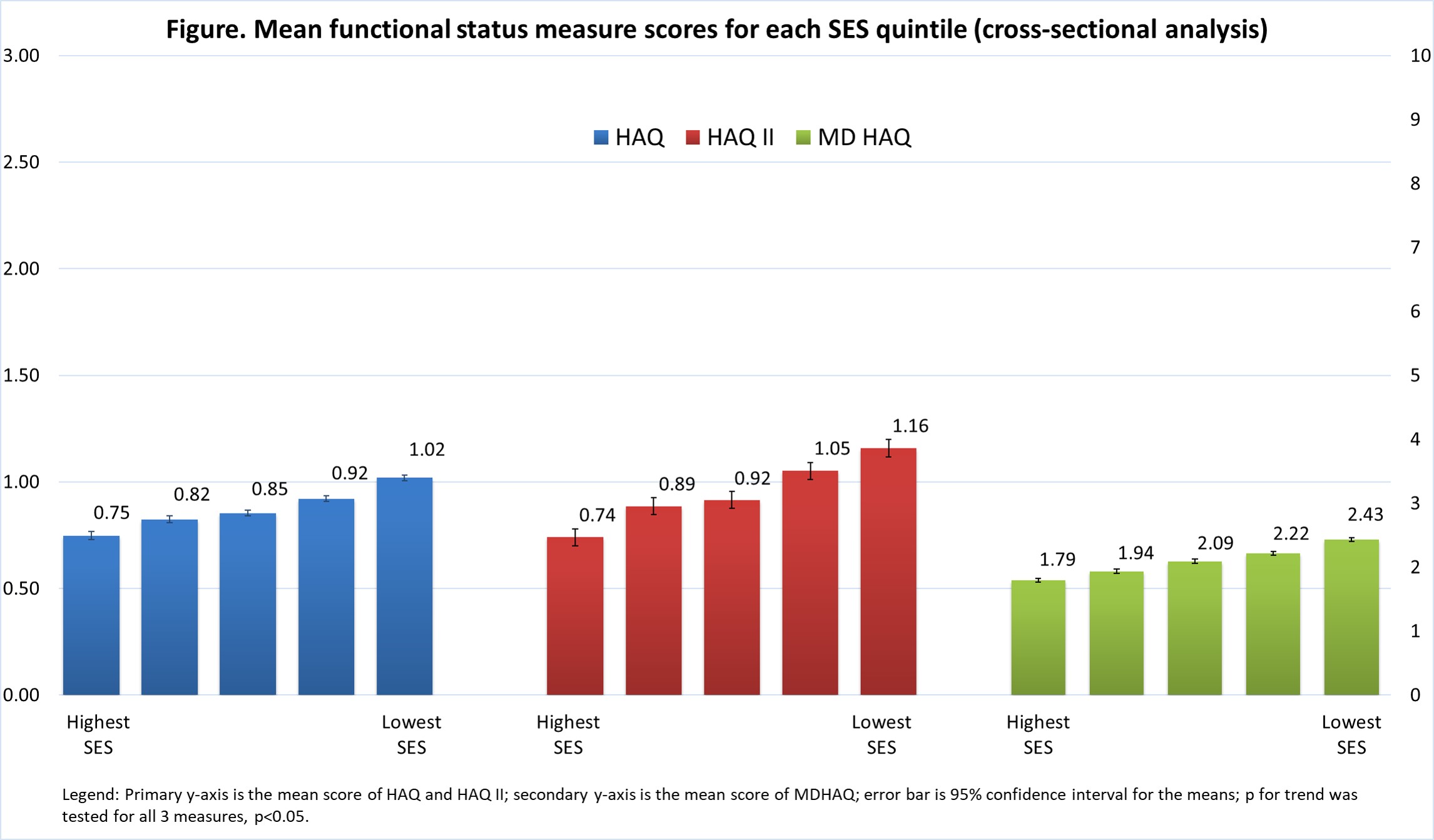
We investigated cross-sectional and longitudinal relationships between FS and SES. In a cross-sectional analysis, we calculated the mean FS scores for each quintile of SES. We used only the most recent FS measure for patients with ≥ 1 score recorded during a calendar year. In a longitudinal analysis, patients with ≥2 of the same FS measure, at least 12 months apart, were categorized as worsening (Y/N) based on the minimal clinically important difference for each tool. We used multi-level logistic regression to assess the association of worsening FS for each quintile of SES, accounting for age, sex, race, baseline FS score, and clustering by practice.
Results: 83,965 patients from 109 practices were included (characteristics in Table). MDHAQ was the most commonly reported FS measure (67.8% of patients), followed by HAQ (24.4%) and HAQII (7.8%). Overall, mean (SD) FS scores for these measures were 2.1 (2.0), 0.89 (0.58), 0.9 (0.6), respectively.
In the cross-sectional analysis, mean FS score was worse at lower SES levels, regardless of the measure used (p-trend< 0.05, see Figure). Among 24,846 RA patients included in the longitudinal analysis with MDHAQ scores, the proportion of patients with a worsening score increased modestly as lower SES levels, even after adjustment (p< 0.05): in the highest SES quintile, 12.7% (95% CI 8.9%-16.5%) patients worsened; in the lowest SES quintile, 16.6% (95% CI 12.1%-21.1%) worsened. The same trend was observed for patients with HAQ and HAQII.
Conclusion: We found evidence of significant disparities in FS across SES in this national cohort of individuals with RA, with worse functional status across each successive lower quintile of SES. In addition, FS declined more rapidly over time in those with lower SES. Future research is needed to identify the source of these disparities, which exist in spite of access to rheumatologic care for all patients in the cohort.
Disclaimer: This data was supported by the ACR’s RISE Registry. However, the views expressed represent those of the authors, not necessarily those of the ACR.
To cite this abstract in AMA style:
Li J, Schmajuk G, Evans M, Izadi Z, Katz P, Ogdie A, Suter L, Yazdany J. Socioeconomic Disparities in Functional Status Among RA Patients: A Longitudinal Analysis Using RISE Data [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/socioeconomic-disparities-in-functional-status-among-ra-patients-a-longitudinal-analysis-using-rise-data/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/socioeconomic-disparities-in-functional-status-among-ra-patients-a-longitudinal-analysis-using-rise-data/