Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: In the US, the COVID-19 pandemic has prompted increased utilization of telemedicine (TM), electronic patient portals (EPPs), and other electronic modalities of health care delivery. Here, we assessed for socioeconomic inequities in TM and EPP utilization in an urban county hospital rheumatology clinic during COVID-19.
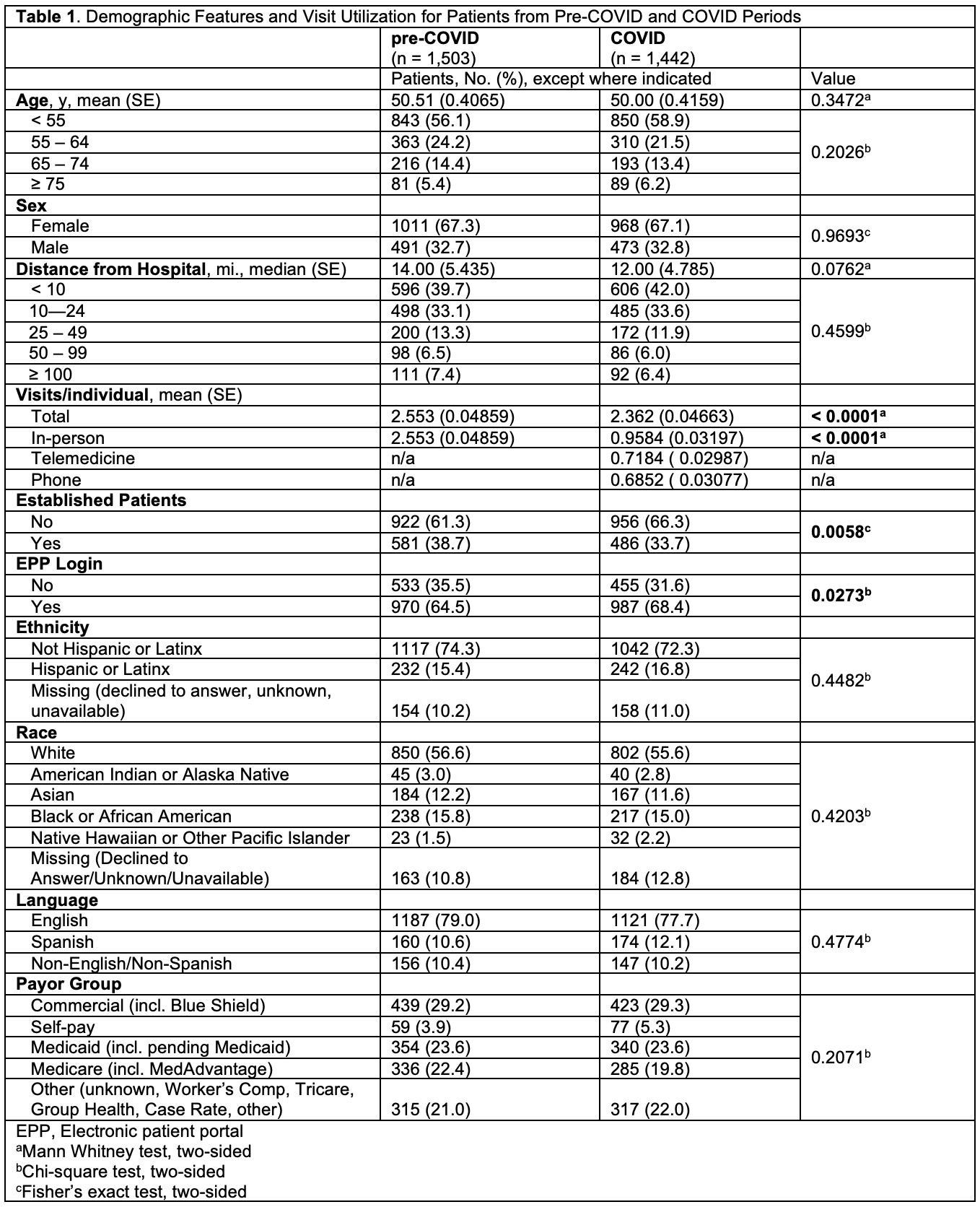
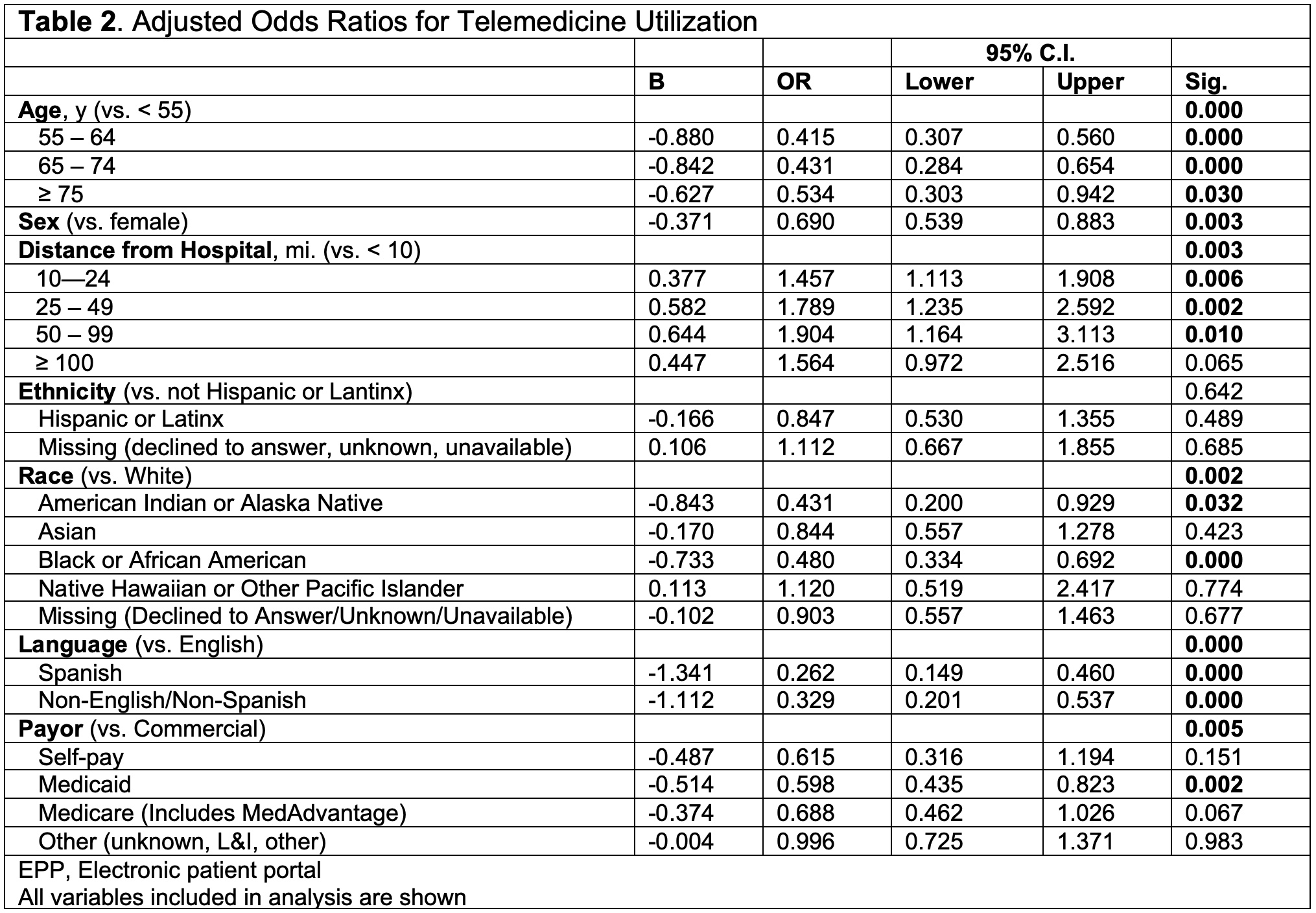
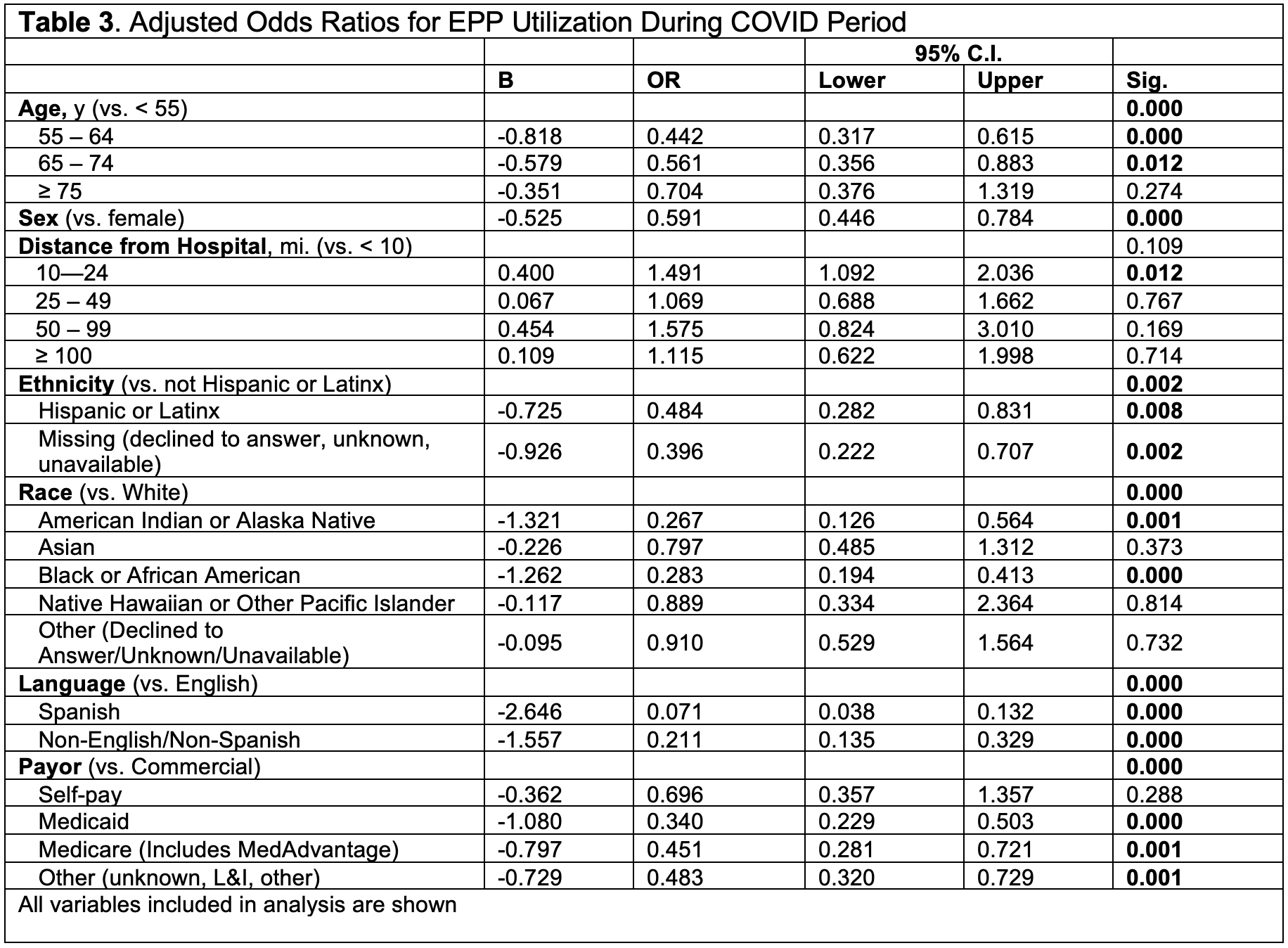
Methods: Using the electronic health record (EHR), demographic features (age, sex, race, ethnicity, language, distance from hospital, payor) on all patients completing visits between 3/1/2019 and 2/28/2020 (pre-COVID period) and 4/1/2020 and 3/31/2021 (COVID period) were analyzed. Bivariate logistic regression analysis was performed to obtain adjusted odds ratios (aORs) for primary outcome (completion of ≥ 1 TM visit during COVID) and secondary outcome (any utilization of the EPP from its inception in 2013 through date of data pull, 4/1/2021).
Results: 1,503 patients completed 3,837 visits in the pre-COVID period (all in-person visits). During COVID, 1,442 patients completed 3,406 visits (40.6% in-person, 20.4% TM, 29.1% telephone visits). 864 patients were seen in both periods. Demographic and visit characteristics are shown in Table 1. During COVID, younger age, farther distance from hospital, female sex, English language preference, White race identity, and commercial payor were associated with TM use (Table 2). White-identifying patients were 2.1x and 2.3x more likely than Black/African-American and American Indian/Alaska Native patients, respectively, to use TM. English-preferring patients were 3.8x and 3.0x more likely than Spanish-preferring and other non-English-preferring patients to use TM, respectively. Among patients seen during COVID, EPP use was associated with younger age, female sex, non-Hispanic/Latinx ethnicity, White race identity, English language preference, and commercial payor (Table 3). White-identifying patients were 3.5x and 3.7x more likely than Black/African-American and American Indian/Alaska Native patients, respectively, to use EPP. English-preferring patients were 14.1x and 4.7x more likely than Spanish-preferring and other non-English-preferring patients to use EPP.
Conclusion: We observed significant age-, sex-, race-, and language-related inequities in TM and EPP use during COVID-19 among patients in an urban county hospital rheumatology clinic. The strongest single predictor of both TM and EPP use was English language preference. Given the growing importance electronic health care delivery, it is critical to identify and address language and socioeconomic barriers to TM and EPP access in order to provide just and equitable rheumatology care.
To cite this abstract in AMA style:
Thomason J, Mantilla B, Bays A, Huang I, hughes G. Socioeconomic Characteristics Associated with Electronic Health Care Utilization in an Urban Rheumatology Clinic During the COVID-19 Pandemic [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/socioeconomic-characteristics-associated-with-electronic-health-care-utilization-in-an-urban-rheumatology-clinic-during-the-covid-19-pandemic/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/socioeconomic-characteristics-associated-with-electronic-health-care-utilization-in-an-urban-rheumatology-clinic-during-the-covid-19-pandemic/