Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Self-efficacy is the belief that one can carry out a behavior necessary to reach a desired goal. A better self-efficacy has been reported as a predictor of better clinical outcomes in SLE patients such as a better HRQoL. However, predictors of a better self-efficacy in SLE patients remain to be identified. The aim of this study is to determine the predictors of a better general self-efficacy in SLE patients.
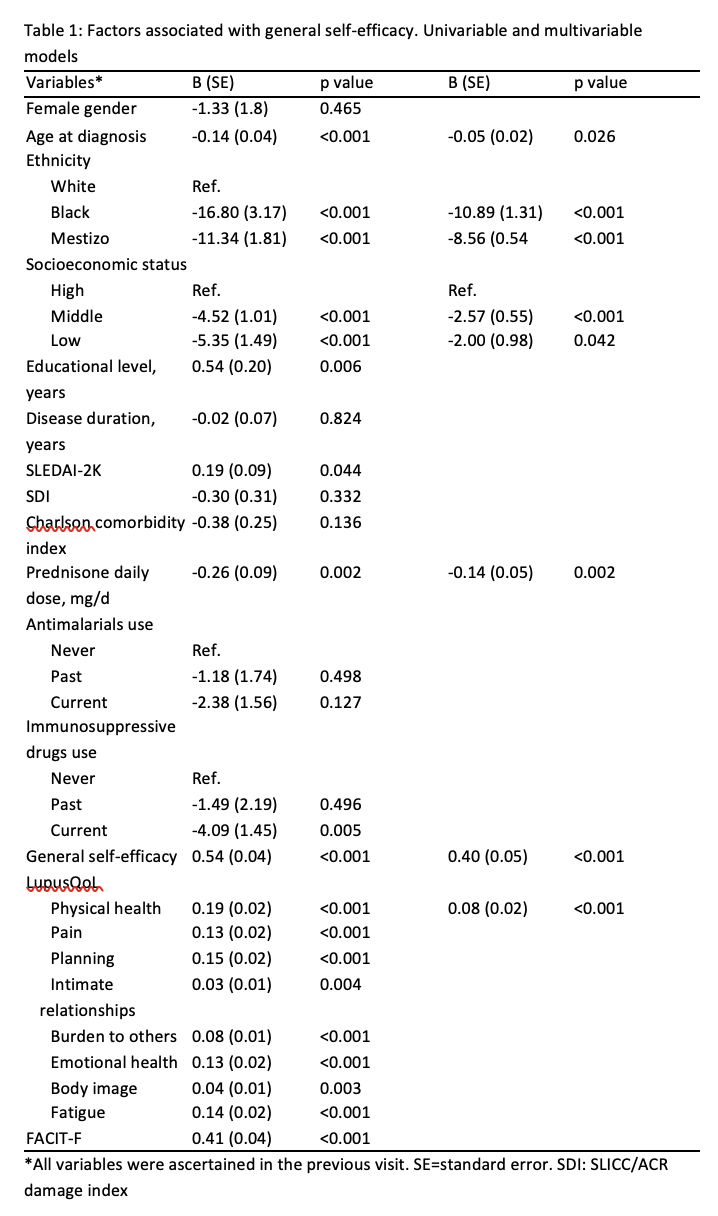
Methods: Patients from a single-center Peruvian lupus cohort were included. General self-efficacy was measured with the Patient-Reported Outcomes Measurement Information System (PROMIS) general self-efficacy instrument. For this instrument, a score of 50 is the average for a clinical population, a higher score indicates a greater self-efficacy. Potential predictors examined were gender, age at diagnosis, ethnicity, socioeconomic status, educational level, disease duration, disease activity (ascertained with the SLEDAI-2K), damage (ascertained with the SLICC/ACR damage index, SDI), Charlson comorbidity index, CS as prednisone daily dose, antimalarials and immunosuppressive drugs use, HRQoL (assessed with the LupusQoL), fatigue (ascertained with the FACIT-F) and previous general self-efficacy. Univariable and multivariable generalized estimating equations (GEEs) were performed using general self-efficacy in the subsequent visit, and the potential predictive factors in the previous visit. A multivariable model was done using a backward selection procedure with an alpha to stay in the model of 0.05.
Results: 820 visits from 274 patients were included; 256 (93.4%) were women with a mean age at diagnosis of 35.5 (13.3) years. General self-efficacy at baseline was 47.0 (10.0) and during the follow-up it was 46.6 (10.1). In the multivariable model, age at diagnosis, non-White ethnicity, lower socioeconomic status and the daily prednisone dose were negatively associated with general self-efficacy; better physical health and previous general self-efficacy were positively associated with general self-efficacy (table 1)
Conclusion: Age at diagnosis, lower socioeconomic status, non-White ethnicity and the daily prednisone dose predicted a worse self-efficacy; a better physical health and previous general self-efficacy predicted a better general self-efficacy. Further studies are needed to define the best strategies to improve general self´-efficacy in SLE patients.
To cite this abstract in AMA style:
Ugarte-Gil M, Gamboa-Cárdenas R, Reategui-Sokolova C, Pimentel-Quiroz V, Elera-Fitzcarrald C, Cucho-Venegas J, Pastor-Asurza C, Rodriguez-Bellido Z, Perich-Campos R, Alarcón G. Sociodemographic Features, Health-Related Quality of Life (HRQoL), Previous General Self-Efficacy and Corticosteroids (CS) Are Associated with General Self-Efficacy in Systemic Lupus Erythematosus (SLE) Patients. Data from a Prevalent Latin American Lupus Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/sociodemographic-features-health-related-quality-of-life-hrqol-previous-general-self-efficacy-and-corticosteroids-cs-are-associated-with-general-self-efficacy-in-systemic-lupus-erythematosus-sl/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sociodemographic-features-health-related-quality-of-life-hrqol-previous-general-self-efficacy-and-corticosteroids-cs-are-associated-with-general-self-efficacy-in-systemic-lupus-erythematosus-sl/