Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Increasing evidence suggests that socioeconomic status drives differences in outcomes for people with rheumatic conditions. Individuals with complex, rare rheumatic conditions such as antineutrophil cytoplasmic antibody (ANCA) vasculitis already struggle to navigate health systems designed to manage common conditions, with fragmented and poorly coordinated care. However, the intersection between these health inequalities and other health determinants is poorly understood. In a national ANCA vasculitis cohort we identified patterns of healthcare use in relation to sociodemographic factors to inform initiatives to address health inequalities.
Methods: The association between non-attendance at outpatient clinics and emergency care episodes (including emergency department attendances and unscheduled hospital admissions) and individual sociodemographic factors were examined in a population-based data linkage study using routine healthcare data obtained from patients with ANCA vasculitis in Scotland between 01/01/2011 and 31/10/2020. Records were linked using unique patient identifiers, pseudonymised, and accessed through the Trusted Research Environment for national datasets in Scotland (eDRIS).
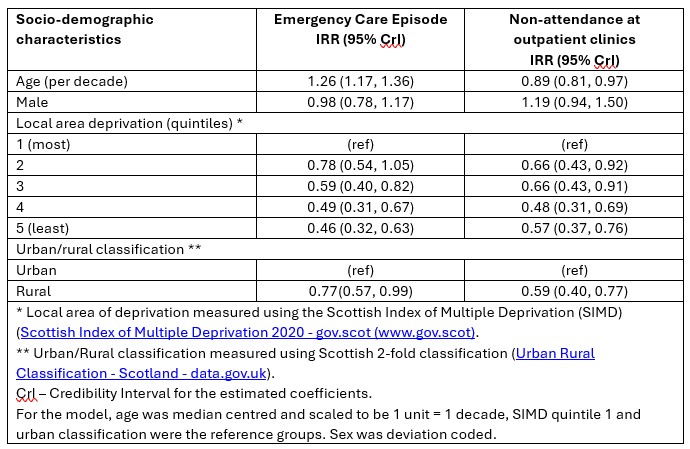
A Bayesian Bivariate Poisson regression was used to estimate rates of emergency care and non-attendance at outpatient clinics per year using duration of follow up (in years) as the exposure term. The model included grouped intercepts by patient to estimate the correlation between the rate of emergency visits and non-attendance, presented as incident rate ratios (IRRs) with 95% credibility intervals. The model was adjusted for age at index date, sex, local area measure of deprivation (quintiles), and the Scottish Government urban rural classification.
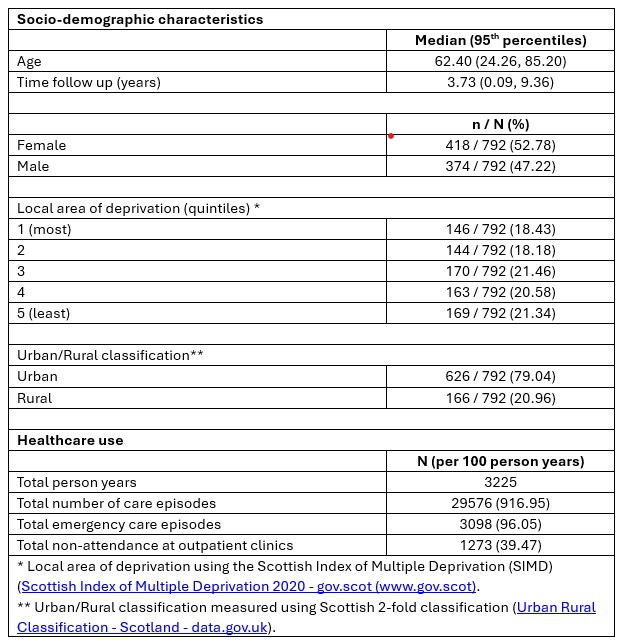
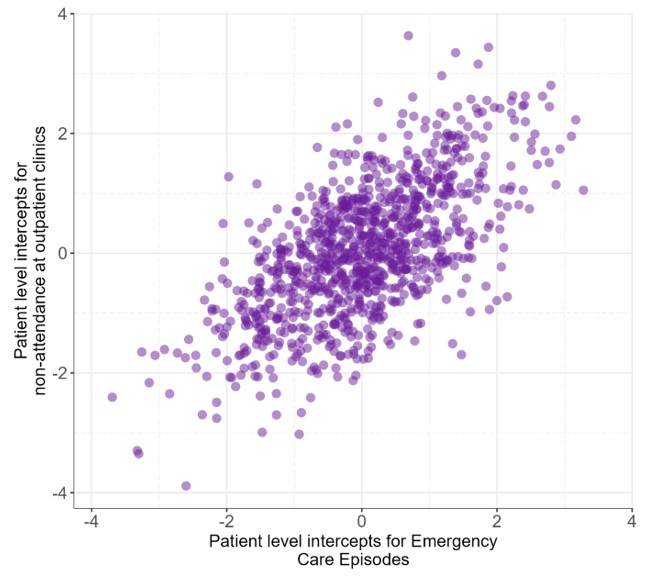
Results: There were 792 patients in this analysis, of whom 52.8% were female with a median age of 62.4 (95th percentiles 24.3 – 85.2), and median follow up of 3.7 years (95th percentiles 0.1 – 9.4), see Table 1. People living in the least deprived areas had fewer emergency care episodes (IRR 0.46, 95% CrI 0.32, 0.63) and missed fewer outpatient appointments (IRR 0.57, 95% CrI 0.37, 0.76) compared to those living in the most deprived areas, see Table 2. Older people tended to have a higher rate of emergency visits (IRR 1.26, 95% CrI 1.17 ,1.36 per decade) but lower rates of missed outpatient appointments (IRR 0.89, 95% CrI 0.81, 0.97, per decade). People living in rural settings had lower rates of both emergency care episodes (IRR 0.77, 95% CrI 0.57, 0.99) and missed appointments (IRR 0.59, 95% CrI 0.40, 0.77) compared to those living in urban settings. Individuals with higher rates of clinic non-attendance tended to have higher rates of emergency care, see Figure 1, with a correlation of 0.65 (95% CrI 0.56, 0.74).
Conclusion: Individual sociodemographic factors associated with higher rates of non-attendance at outpatient clinics and unscheduled care episodes were identified in a national ANCA vasculitis cohort. Identifying those who may struggle to access care and for whom care is more fragmented and unplanned will help inform delivery of more equitable person-centred models of care for those with ANCA vasculitis and other rare autoimmune rheumatic conditions.
To cite this abstract in AMA style:
James W, Black C, Basu N, Little M, Hollick R. Sociodemographic Factors Associated with Clinic Non-attendance and Unscheduled Emergency Care Episodes in ANCA-associated Vasculitis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/sociodemographic-factors-associated-with-clinic-non-attendance-and-unscheduled-emergency-care-episodes-in-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sociodemographic-factors-associated-with-clinic-non-attendance-and-unscheduled-emergency-care-episodes-in-anca-associated-vasculitis/