Session Information
Date: Tuesday, November 7, 2017
Title: ARHP: Exemplary Abstracts
Session Type: ARHP Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Cognitive Dysfunction (CD) is seen among 20-80% of patients with Systemic Lupus Erythematosus (SLE) and adversely affects their quality of life and productivity. Pain, a known correlate of CD, may occur in SLE from the disease itself or concurrent fibromyalgia (FM). Sleep issues and depression, also encountered in SLE, may impact both pain and CD. With the goal of a potential intervention for CD, we explored whether sleep issues and depression mediated the relationship between pain and CD in SLE patients.
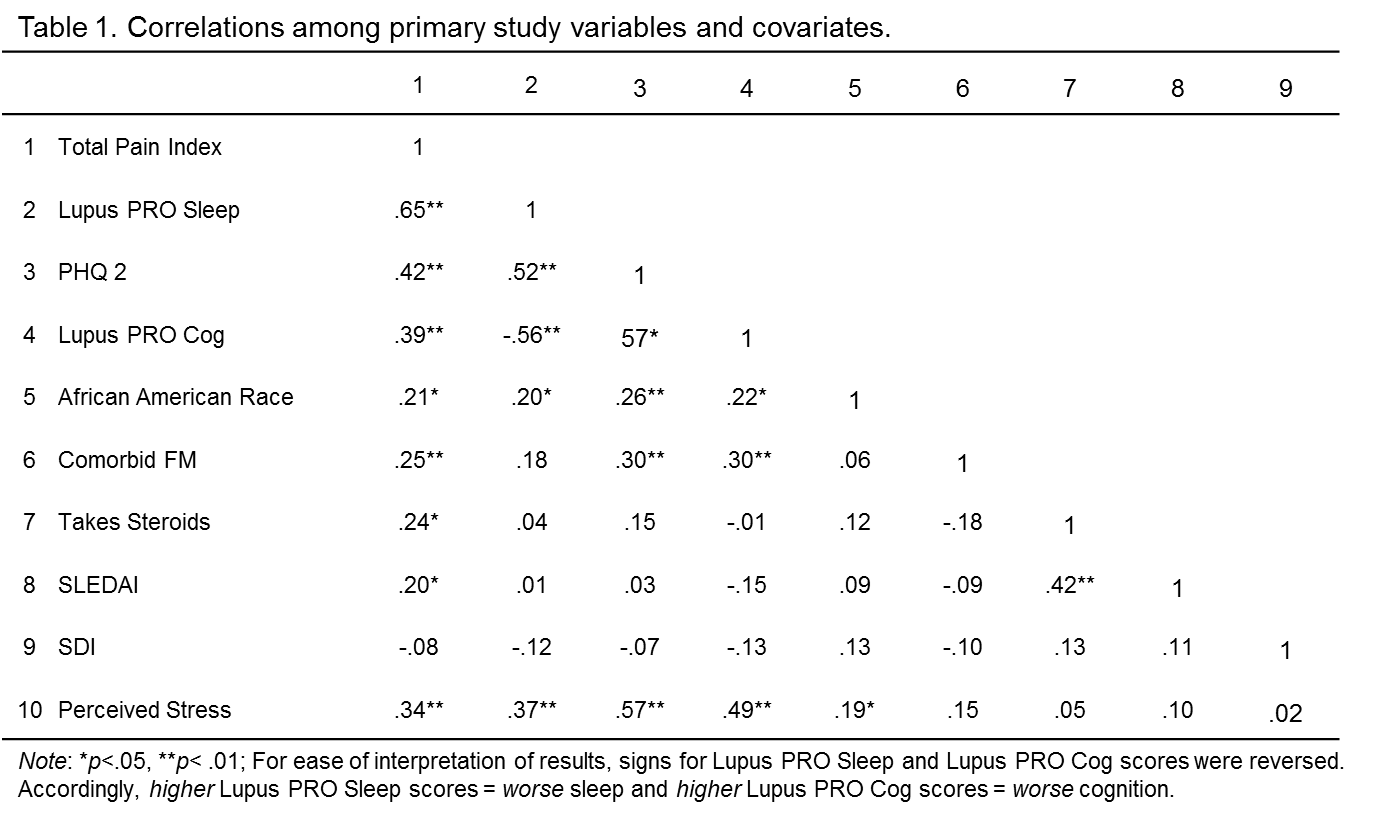
Methods: 115 consenting SLE patients were recruited from a Rheumatology outpatient clinic. Patients completed questionnaires on demographics, pain (Pain Inventory), stress [(Perceived Stress Scale (PSS)], depression (PHQ2), sleep (LupusPROv1.8), and cognition (LupusPROv1.8). Diagnosis of concurrent FM and current steroid use were identified via chart review. Physicians performed disease activity (SELENA-SLEDAI) and damage (SLICC-ACR/ SDI) assessment. Bivariate correlations were used to determine relationships between above variables. Relationships among pain, sleep, depression and CD (primary variables) were assessed with bootstrapped mediation models controlling for race/ethnicity, FM status, current steroid use, SLEDAI, SDI, and stress (covariates).
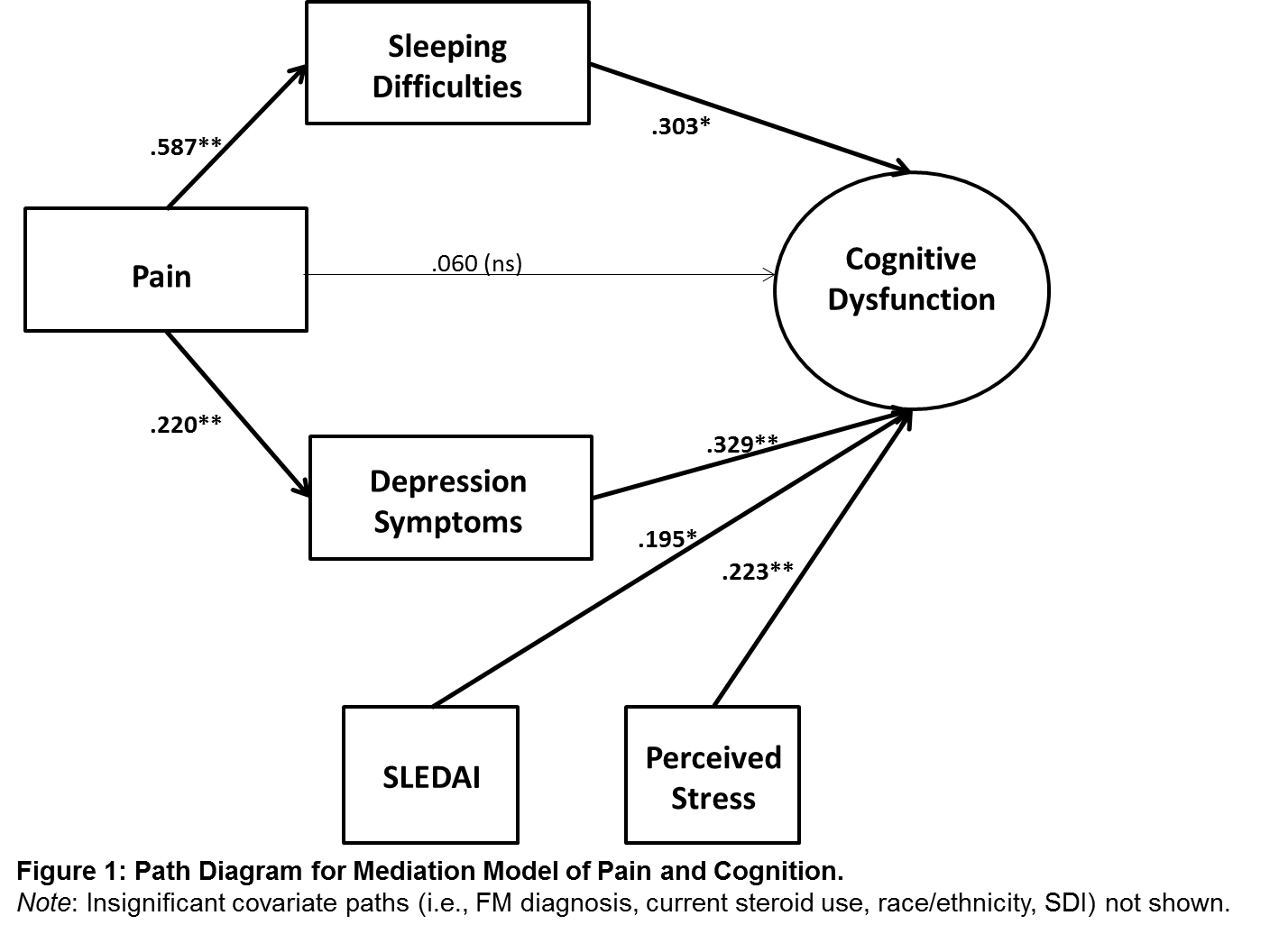
Results: The sample was 90% female: average age was 40 years (SD 13). Racial composition was 52% African-American, 24% White, 11% Hispanic, 5% Asian, and 8% other. There were significant relationships noted among the variables (Table 1), including a positive relationship between pain and CD (r 0.39). Mediation analyses (Figure 1) indicated that the effect of pain on CD was mediated by depression (B 0.33) and sleep (B 0.30). These effects were maintained even after controlling for aforementioned covariates, of which, only SLEDAI (B 0.20) and stress (B.22) were significantly linked to CD [all p’s < .05] in the full model.
Conclusion: Even after controlling for disease activity and stress, both sleep and depression accounted for the relationship between pain and CD in SLE. These relationships need validation in longitudinal studies with additional measurement modalities. Our findings indicate promising, non-pharmacologic intervention avenues for SLE patients with pain and CD. Cognitive-behavioral therapies for depression and sleep are known to reduce distress and enhance functioning across various psychosocial domains. Given the symptom burden of SLE, interventions that maximize potential benefits without additional pharmacologic treatments may be of particular utility.
To cite this abstract in AMA style:
Lillis TA, Tirone V, Weinberg S, Gandhi N, Nika A, Sequeira W, Hobfoll SE, Block JA, Jolly M. Sleep and Depression Mediate the Relationship between Pain and Cognitive Dysfunction in Lupus Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/sleep-and-depression-mediate-the-relationship-between-pain-and-cognitive-dysfunction-in-lupus-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sleep-and-depression-mediate-the-relationship-between-pain-and-cognitive-dysfunction-in-lupus-patients/