Session Information
Date: Monday, October 22, 2018
Title: 4M087 ACR Abstract: Reproductive Issues in Rheumatic Disorders (1852–1857)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Systemic lupus erythematosus (SLE) disproportionally affects women of childbearing age. Low disease activity for 6 months prior to conception leads to the best outcomes; however, there is little prospective data describing the relative frequency and predictors of flares during and after pregnancy under such conditions.
Methods:
Analyses used data from the PROMISSE study, a multicenter, prospective observational study (2003-2014) of 384 pregnant women meeting ≥ 4 ACR SLE criteria. Subjects were enrolled <12wks gestation and samples collected throughout pregnancy and post-partum. Exclusion criteria were multi-fetal pregnancy, active disease (prednisone >20mg/d), or renal disease (proteinuria >1gm/24h, and creatinine > 1.2mg/dL). Mild/moderate and severe flares were defined using the SELENA-SLEDAI Flare Index. Flares during pregnancy were assessed in all 384 patients, and post-partum flares in those with study visits 2-6 months post-partum. Logistic regression models were fit to the data to identify independent predictors of experiencing any type of flare during pregnancy and post-partum.
Results:
Rates of Flare:
105 flares were recorded during pregnancy (3.8% 1st Trimester, 53.3% 2nd, 42.9% 3rd). Counting one flare per person, 100 of 384 patients (26%) flared at any point during pregnancy; 20.8% of patients had mild/moderate flares and 6.25% had severe. 57 of 234 patients (24.4%) with a study visit 2-6 months post-partum flared; 22.7% had mild/moderate flares and 1.7% severe. Post-partum flares were mild, and 19 of 57 (33.3%) were treated; 13 with an increase in prednisone, 6 with NSAID or hydroxychloroquine, and 1 with mycophenolate mofetil. The rate of any type of flare was 0.39/person-year at any point during pregnancy and 0.84/person-year post-partum. The proportion of subjects who had any flares during and after pregnancy was similar, but the post-partum flares occurred over a shorter duration of follow-up.
Correlates of Flare:
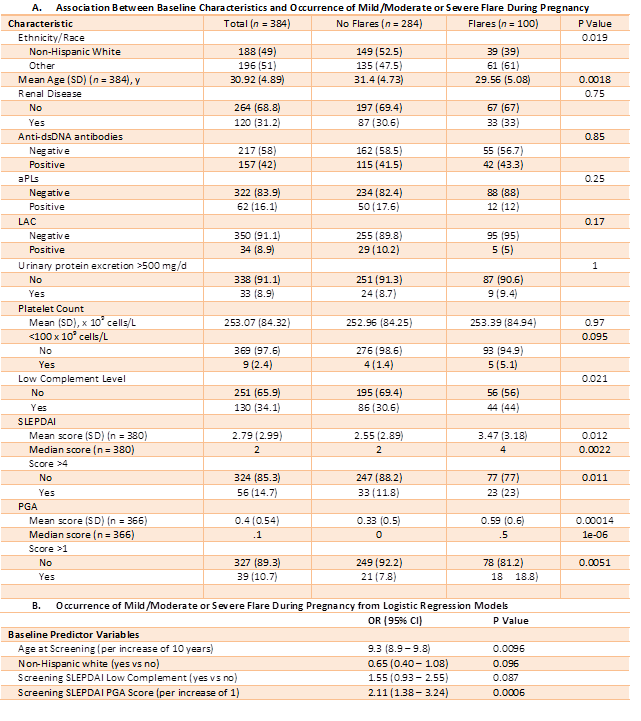
Among baseline variables considered (Table) only age, ethnicity/race, low complement, and PGA were independently predictive of having any flare during pregnancy. Clinical features associated with adverse pregnancy outcome (platelet count, antihypertensive use, and LAC) were not predictive of flare. The mean time from the last visit during pregnancy to the post-partum visit was 20 weeks and ranged from 9 to 34 weeks. Neither baseline clinical variables nor clinical variables of the last visit during pregnancy were associated with occurrence of any post-partum flare.
Conclusion:
Flares during pregnancy are correlated with clinical and serological activity during the first trimester. Flares during and after pregnancy are typically mild, infrequently require treatment, and occur at similar rates.
To cite this abstract in AMA style:
Davis-Porada J, Stern S, Guerra MM, Laskin C, Petri M, Lockshin M, Sammaritano LR, Branch D, Sawitzke AD, Merrill JT, Buyon JP, Kim M, Salmon JE. SLE Flares during and after Pregnancy Are Mild and Occur at Similar Rates [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/sle-flares-during-and-after-pregnancy-are-mild-and-occur-at-similar-rates/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sle-flares-during-and-after-pregnancy-are-mild-and-occur-at-similar-rates/