Session Information
Date: Monday, November 13, 2023
Title: (1013–1032) Healthcare Disparities in Rheumatology Poster II: Socioeconomic Determinants
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Access to care varies across health systems. Countries with universal health insurance are thought to have less wealth-based health disparities, but it is unclear if this applies to total hip arthroplasty (THA) utilization and outcomes. The purpose of this study was to determine whether a single-payer healthcare system would mitigate income-based disparities in THA utilization and outcomes.
Methods: We retrospectively compared all patients undergoing THA from 1/2012 to 9/2018 in Ontario (ON), Canada and Pennsylvania (PA), United States. We obtained PA patient data from Pennsylvania Health Care Cost Containment Council and ON patient data from Ontario’s Institute for Clinical Evaluative Sciences. Patient-level data were linked to Census data of median household income of the ZIP code or postal code of patients’ residence. We then analyzed whether community income-based differences in THA utilization were reduced in Ontario compared to Pennsylvania due to Canada’s single-payer healthcare system. We used logistic regression to examine the relative risks for lowest community income of outcomes such as rates of 1-year revision, 90-day mortality, and 90-day readmission in the two regions.
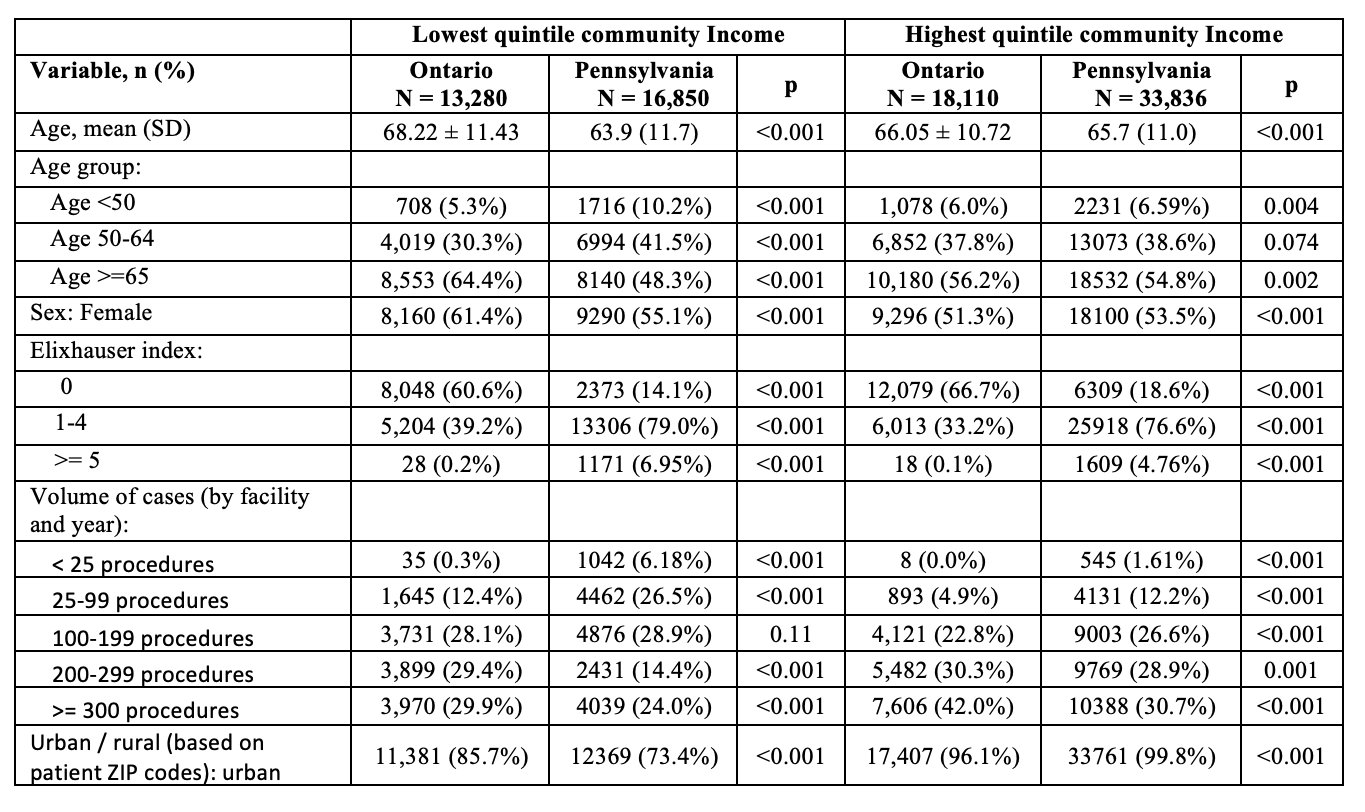
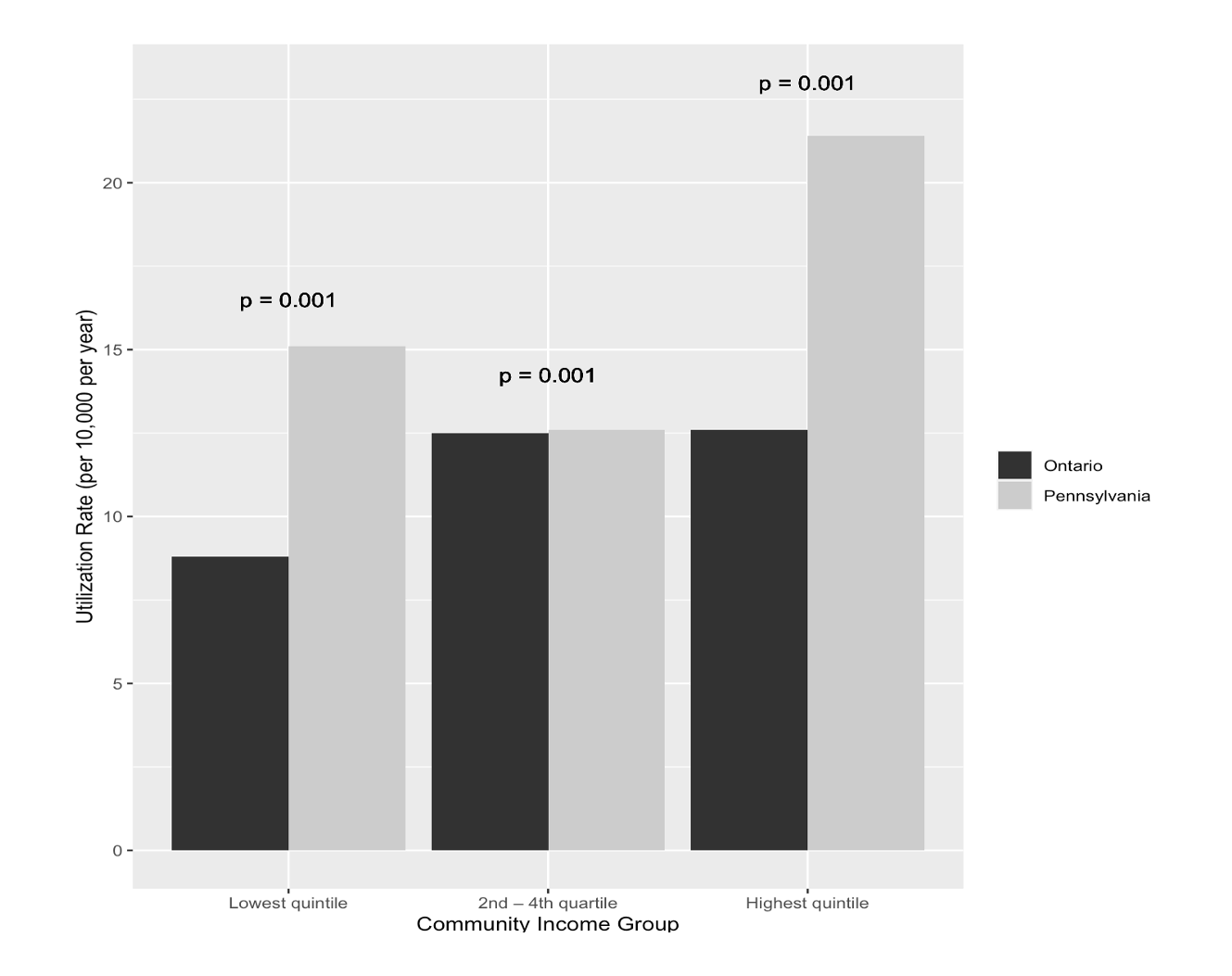
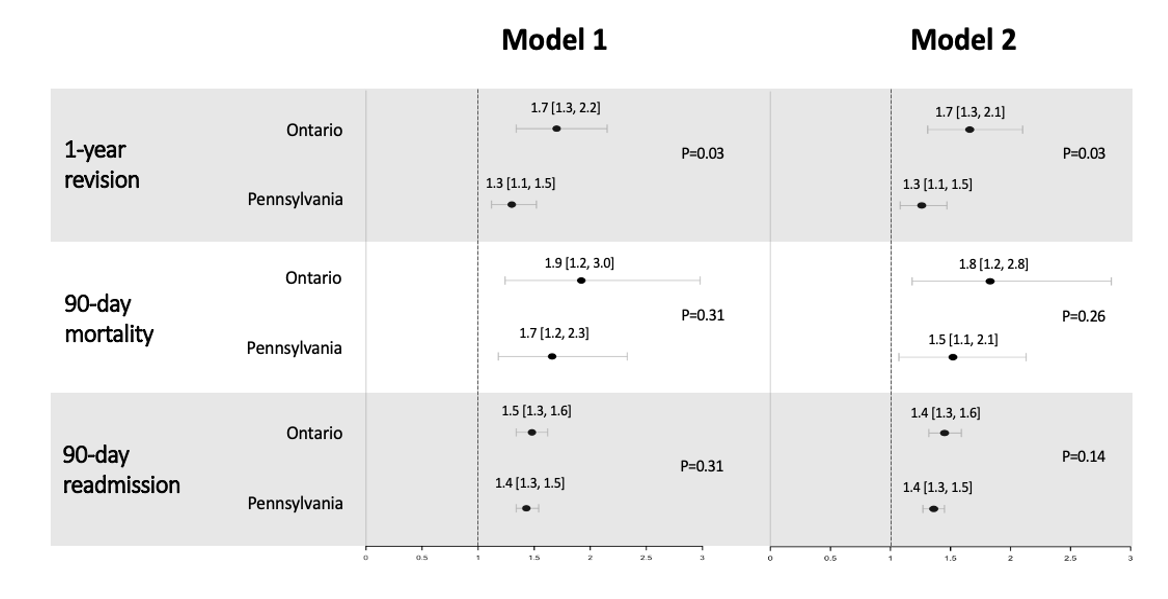
Results: Among all THAs, 13,280 patients (15.8%) and 16,850 patients (16.0%) lived in communities within the lowest income quintile in Ontario and Pennsylvania, respectively (Table 1). Overall THA utilization was lower in Ontario compared to Pennsylvania across income groups (Figure 1). In Ontario, patients in the highest income quintile utilized THA 43.2% more than those in the lowest income quintile (12.6 vs 8.8); this difference in utilization was slightly greater than the difference in Pennsylvania, where patients in the highest income quintile utilized THA 41.7% more than patients in the lowest income quintile (21.4 vs. 15.1) (p < 0.001). Patients in the lowest community income quintile in Pennsylvania had a greater rate of 1-year revision, 90-day mortality, and 90-day readmission compared to patients in the lowest income quintile of Ontario. However, after adjusting for age, sex, hospital volume, and rural vs. urban hospital, the odds for patients in the lower-income group compared to the higher-income group of 1-year revision (ON: OR 1.70, 95% CI: [1.34, 2.15]. PA: 1.30 [1.12, 1.52]), 90-day mortality (ON: 1.92 [1.24, 2.98]. PA: 1.66 [1.18, 2.33]), and 90-day readmission (ON: 1.48 [1.34, 1.62]. PA: 1.43 [1.34, 1.54] were greater in Ontario compared to Pennsylvania (Figure 2).
Conclusion: Income-based differences in THA utilization were greater in Ontario than in Pennsylvania. Additionally, patients in low-income communities in Ontario were at greater risk relative to higher community income patients for adverse outcomes. These findings suggest that a single-payer insurance system may not be sufficient to eliminate income-based differences in utilization and complications of THA.
Note: Model 1 adjusts for income group, age, sex, hospital volume, rural / urban hospital. Model 2 adjusts for income group, age, sex, hospital volume, rural / urban hospital, and Elixhauser index.
To cite this abstract in AMA style:
Mehta B, Ho K, Gibbons J, Ling V, Goodman S, Parks M, Ravi B, Wang F, Ibrahim S, cram P. Single-Payer Health Insurance May Not Mitigate Income-Based Differences in Total Hip Arthroplasty Utilization: A Transnational Analysis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/single-payer-health-insurance-may-not-mitigate-income-based-differences-in-total-hip-arthroplasty-utilization-a-transnational-analysis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/single-payer-health-insurance-may-not-mitigate-income-based-differences-in-total-hip-arthroplasty-utilization-a-transnational-analysis/