Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Degenerative changes of the spine (DC), diffuse idiopathic skeletal hyperostosis (DISH) and radiographic axial Spondyloarthritis (r-axSpA) may present with overlapping inflammatory and degenerative findings on imaging, which, next to the general symptom of chronic back pain might, represent a challenge for an accurate diagnosis. We aimed to evaluate the distribution of spinal imaging features in a real-life cohort of patients with chronic back pain referred to a tertiary university rheumatology center and identify those associated with DC, DISH or r-axSpA.
Methods: In a cross-sectional analysis of patients with chronic low back pain, demographic and disease data were collected. Imaging of the spine (thoracic or lumbar) and sacroiliac joints was performed per the clinical indication. All images were evaluated by two independent trained readers including erosions, sclerosis, squaring, osteophytes and syndesmophytes on conventional radiographs (CR) and bone marrow edema (BME) or degenerative changes on magnetic resonance imaging (MRI). The final diagnosis made by the rheumatologist at discharge was the gold standard. Data were presented descriptively and compared among the three diagnosis groups (DC, DISH and axSpA).
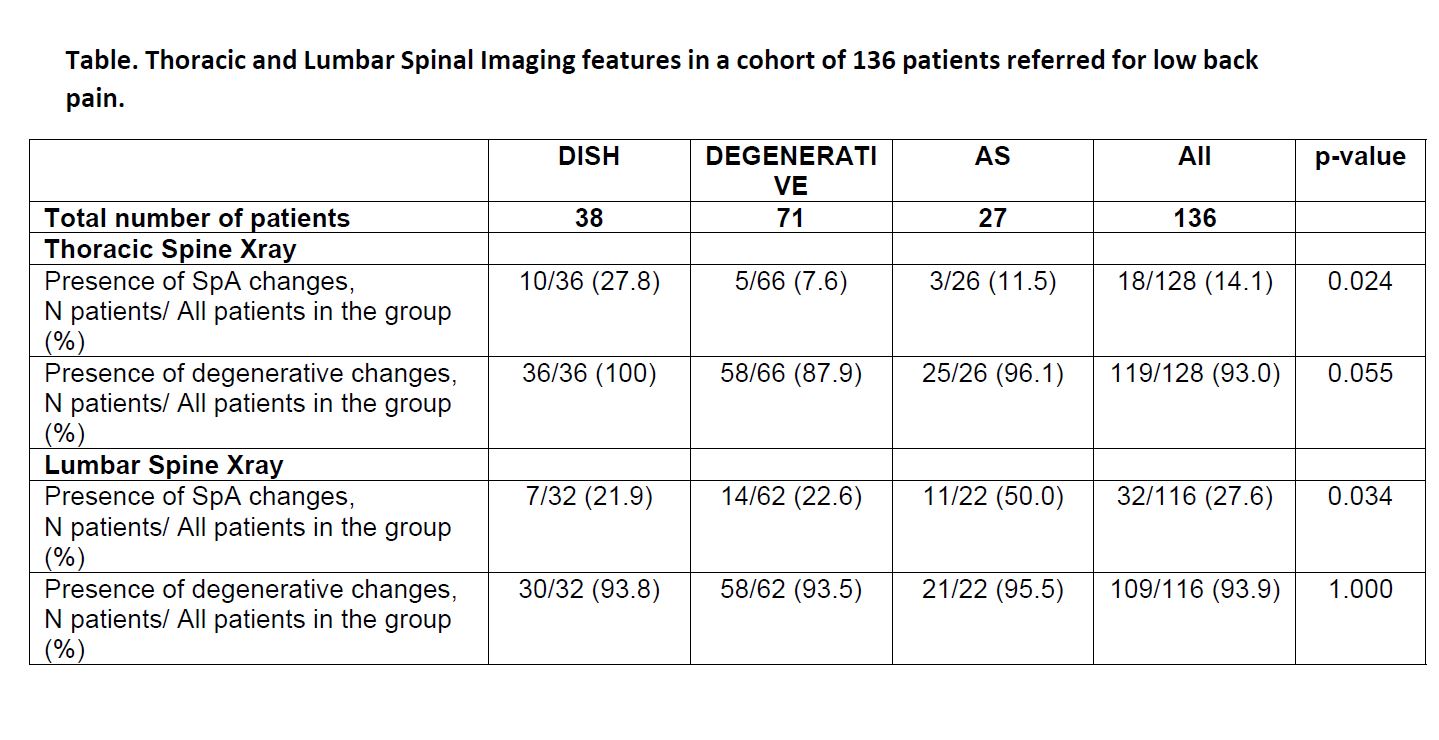
Results: Among 136 referred patients, 71 had DC, 38 DISH, and 27 r-axSpA. Mean age was 63.2±11.4 (p=0.135 among the three groups), and 86 (63.2%) were males (88.9% in axSpA, p=0.003). Patients had high levels of comorbidities: 91 (72.8%) had hypertension (higher in the DC group, 52 (82.8%), p=0.04), 37 (27.6%) had diabetes (higher in DISH, 39.5%, p=0.012) and 31 (23.3%) were current smokers (higher in axSpA, 53.8%, p< 0.001). Although axSpA-related spinal changes on CR were expectedly more prevalent in the axSpA group (thoracic 14.1%, p=0.024; lumbar 93.9%, p=0.034), they were also present in DISH (27.8% and 21.9%) and DC (7.6% and 22.6%, respectively). DC were present in the three groups in 93.0% in the thoracic and in 93.9% in the lumbar spine, without a statistically significant differences (Table). Similarly, on thoracic and lumbar spine MRI, BME was present in DISH in 33.3% and 41.7% and in DC in 20.4% and 32.7% lumbar spines, respectively.
Conclusion: A significant overlap of inflammatory and degenerative features on spinal imaging among patients with DC, DISH or axSpA was found in this older group of patients. Particularly, r-axSpA-related spinal CR features were found in a fourth of patients with DISH, while MRI BME was found in a third of them.
To cite this abstract in AMA style:
Ziade N, Kougkas N, Udod M, Tsiami S, Baraliakos X. Significant Overlap of Inflammatory and Degenerative Features on Spinal Imaging Among Patients with Degenerative Spinal Disease, Diffuse Idiopathic Skeletal Hyperostosis and Radiographic Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/significant-overlap-of-inflammatory-and-degenerative-features-on-spinal-imaging-among-patients-with-degenerative-spinal-disease-diffuse-idiopathic-skeletal-hyperostosis-and-radiographic-axial-spondyl/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/significant-overlap-of-inflammatory-and-degenerative-features-on-spinal-imaging-among-patients-with-degenerative-spinal-disease-diffuse-idiopathic-skeletal-hyperostosis-and-radiographic-axial-spondyl/