Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: A few reports have evaluated the frequency of antiphospholipid antibodies (aPL) in Sjogren’s disease (SjD) and their association with SjD or Antiphospholipid Antibody Syndrome (APS) manifestations. Some authors have suggested an association between presence of aPL and peripheral neuropathy, hypergammaglobulinemia, stroke, and venous thrombosis. Our aim was to assess the frequency of aPL detected in a cohort of well-characterized SjD patients and determine their correlation with key phenotypic features of SjD and clinical manifestations of APS.
Methods: We performed a retrospective chart review of 117 consecutive patients seen at SjD specialty clinic at the University of Kansas Medical Center meeting the 2016 ACR/EULAR classification criteria for SjD who were tested for aPL. All patients underwent testing for anti-cardiolipin antibodies (ACL) IgG/IgM, anti-beta-2-glycoprotein-1 antibodies (B2GP-1) IgG/IgM, and lupus anticoagulants, including Dilute Russell’s Viper Venom Time (DRVVT) and hexagonal phase phospholipid neutralization assay (HPPNA). Clinical, laboratory, and histological manifestations of both SjD and APS were collected. Statistical analyses included Chi-squared, Fisher’s exact test, and Student t-tests, as appropriate.
Results: 103 patients (88%) were females, mean age was 54.6 +/- 13.9 years, 100 patients (85%) were white, and mean disease duration was 2.9 years. Of the 117 SjD patients, 16 (13.7%) had at least one positive testing for antiphospholipid antibodies (Table 1). Only 3 patients (2.5%) met criteria for APS. Detection of aPL was associated with monoclonal gammopathy (56.25% of aPL-positive vs 22.77% of aPL-negative, p = 0.012) and arterial thrombosis (12.5% vs 0%, p = 0.02). We did not observe any other association with clinical, laboratory, or histological parameters (Table 2). Of the 16 patients with positive aPL, 5 patients (31%) had aPL positivity confirmed at least 12 weeks apart whereas 11 patients (69%) had aPL checked only once. There was no association between the number of occurrences of aPL positivity and monoclonal gammopathy (46% of one-time aPL positive vs 80% of two time-aPL positive, p = 0.31) or arterial thrombosis (1% of one-time aPL positive vs 20% of two-time aPL positive, p = 1).
Conclusion: A minority of patients with SjD had aPL and an even smaller group met the criteria for APS. Detection of aPL was associated with the presence of monoclonal gammopathy and arterial thrombosis. Larger studies are necessary to determine the clinical significance and utility of screening for antiphospholipid antibodies in SjD, particularly in those with monoclonal gammopathy.
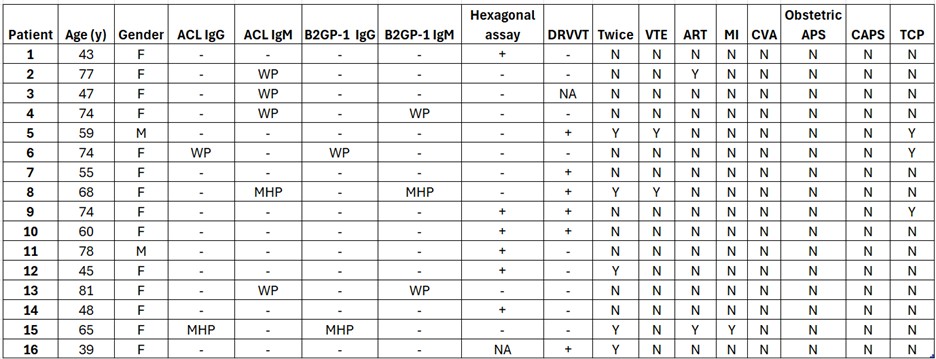 Table 1. 16 SjD patients with positive aPL. F = female, M = male, WP = weakly positive (25-39.9 GPL), MHP = moderate-high positive (> 40 GPL), NA = not available, N = No, Y = Yes, VTE = venous thromboembolism, ART = arterial thrombosis, MI = myocardial infarction, CVA = cerebrovascular accident, CAPS = catastrophic antiphospholipid syndrome, TCP = thrombocytopenia, (+) = positive test, (-) = negative test.
Table 1. 16 SjD patients with positive aPL. F = female, M = male, WP = weakly positive (25-39.9 GPL), MHP = moderate-high positive (> 40 GPL), NA = not available, N = No, Y = Yes, VTE = venous thromboembolism, ART = arterial thrombosis, MI = myocardial infarction, CVA = cerebrovascular accident, CAPS = catastrophic antiphospholipid syndrome, TCP = thrombocytopenia, (+) = positive test, (-) = negative test.
.jpg) Table 2. Features of SjD and APS by aPL status. ILD = interstitial lung disease, LAD = lymphadenopathy, PNS = peripheral nervous system, CNS = central nervous system, MGUS = monoclonal gammopathy of uncertain significance, TCP = thrombocytopenia, VTE = venous thromboembolism, ART = arterial thrombosis, MI = myocardial infarction, CVA = cerebrovascular accident.
Table 2. Features of SjD and APS by aPL status. ILD = interstitial lung disease, LAD = lymphadenopathy, PNS = peripheral nervous system, CNS = central nervous system, MGUS = monoclonal gammopathy of uncertain significance, TCP = thrombocytopenia, VTE = venous thromboembolism, ART = arterial thrombosis, MI = myocardial infarction, CVA = cerebrovascular accident.
To cite this abstract in AMA style:
Thimmapuram R, Alkhatib A, Baker J, Maz M, Noaiseh G. Significance of Antiphospholipid Antibodies in Patients with Sjogren’s Disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/significance-of-antiphospholipid-antibodies-in-patients-with-sjogrens-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/significance-of-antiphospholipid-antibodies-in-patients-with-sjogrens-disease/
