Session Information
Date: Monday, November 13, 2023
Title: (1200–1220) Patient Outcomes, Preferences, & Attitudes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Women with PsA have more severe disease activity and lower health-related quality of life vs men.1 This post hoc analysis assessed sex differences in disease impact perceptions and physician interactions with patients (pts) with PsA using global survey data.
Methods: An online survey by The Harris Poll (Nov 2, 2017–Mar 12, 2018) included 1,286 pts from 8 countries, aged ≥ 18 years, who had PsA for > 1 year, visited a rheumatologist/dermatologist in the past 12 months, and had used ≥ 1 DMARD for PsA.2 Results were stratified post hoc by sex; analyzed descriptively and by binomial (chi-squared) tests. Percentages/binomial tests of the final global data were adjusted for size of each country’s adult population. Statistically significant differences (p < 0.05) were described as more/higher.
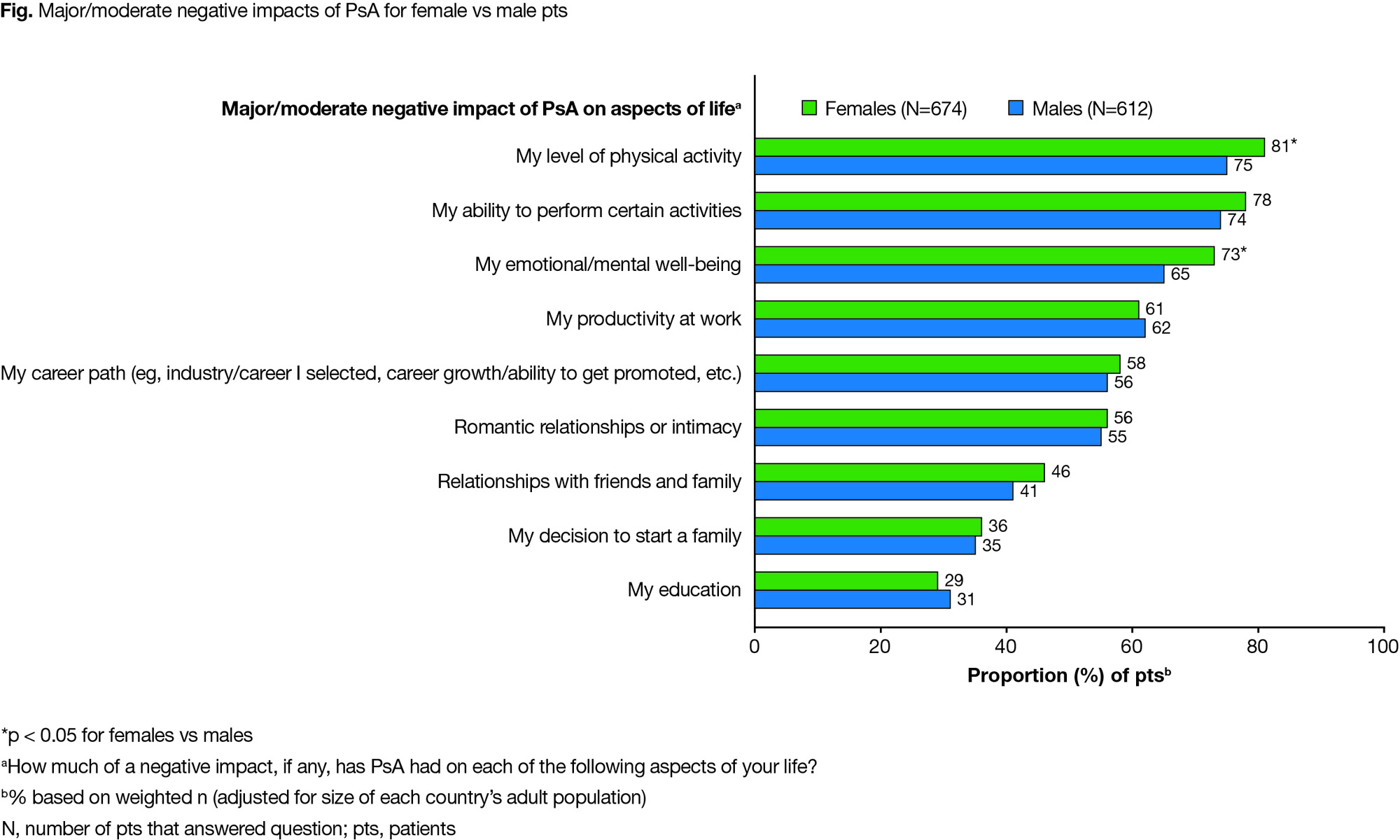
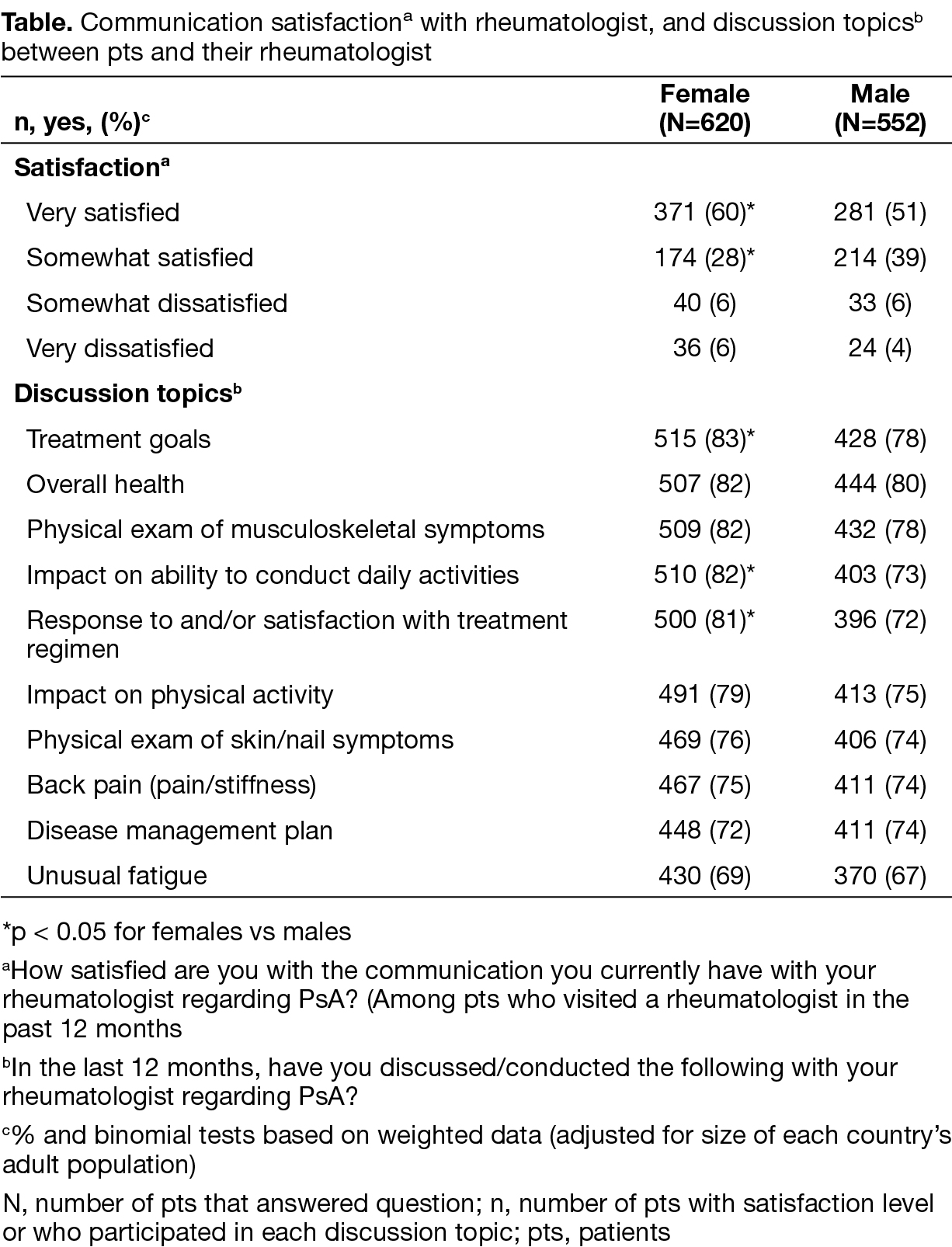
Results: 52% of pts were female; 24% from Europe (France/Spain/UK). Mean age of females/males (41.3/41.0 years) and time since diagnosis (9.2/8.8 years) were similar. More females had anxiety (32% vs 24%), osteoarthritis (17% vs 9%), had taken a steroid (57% vs 43%), and were taking any DMARD (biologic and oral DMARDs; 20% vs 15%). More females vs males reported a major/moderate negative PsA impact on physical activity (81% vs 75%) and emotional/mental well‑being (73% vs 65%); major/moderate impact on other life aspects, such as work productivity, was similar between sexes (Fig). More females vs males reported the following because of PsA: emotional distress (65% vs 50%), stopped social activities (49% vs 41%), and went on permanent work disability (14% vs 9%); more males vs females reported lower work productivity (47% vs 38%) because of PsA. Switching treatment due to joint symptoms (41% vs 28%) and side effects (35% vs 22%) were higher in females vs males; switching due to potential serious side effect concerns (29% vs 16%) and symptoms being under control (18% vs 9%) were higher in males vs females. More females vs males were very satisfied with their rheumatologist’s communication (60% vs 51%), and discussed treatment goals (83% vs 78%), impact on ability to conduct daily activities (82% vs 73%), and response to and/or satisfaction with treatment regimen (81% vs 72%; Table). Pt ability to describe their PsA diagnosis/recall symptoms may limit the study.
Conclusion: More women vs men reported a major/moderate PsA impact on physical and emotional/mental well‑being. More women were very satisfied with communication and discussed treatment goals with their rheumatologist. It is important to consider how sex impacts a pt’s experience with PsA.
- Orbai et al. Arthritis Care Res 2020; 72: 1772–9
- Coates et al. Health Qual Life Outcomes 2020; 18: 173
Study sponsored by Pfizer. Medical writing support provided by LC Rodgers, CMC Connect; funded by Pfizer.
To cite this abstract in AMA style:
Eder L, Richette P, Coates L, Azevedo V, Cappelleri J, Hoang M, Moser J, Kessouri M. Sex Differences in Perceptions of Psoriatic Arthritis Disease Impact, Management, and Physician Interactions: Results from a Global Patient Survey [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/sex-differences-in-perceptions-of-psoriatic-arthritis-disease-impact-management-and-physician-interactions-results-from-a-global-patient-survey/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-differences-in-perceptions-of-psoriatic-arthritis-disease-impact-management-and-physician-interactions-results-from-a-global-patient-survey/