Session Information
Date: Monday, November 6, 2017
Title: Rheumatoid Arthritis – Clinical Aspects II: Treatment Patterns
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Despite a decline in the incidence of orthopedic surgeries for rheumatoid arthritis (RA) in recent years, joint replacement remains an option for patients with treatment refractory disease seeking symptomatic relief and functional improvement. Although multiple factors influence the need for joint surgery in RA, it is unclear if there are sex differences in the incidence and trends of large versus small joint surgery rates in RA over time.
Methods: A retrospective medical record review was performed of all orthopedic surgeries following first fulfilment of 1987 ACR criteria for adult-onset RA in 1980-2013 among residents of a geographically defined area with follow up until death, migration or July 1, 2016. Surgeries were classified as small (wrist, hand, foot) or large (shoulder, elbow, hip, knee, ankle) joint. Trends in incidence of joint surgeries over time by sex were examined using Poisson regression models.
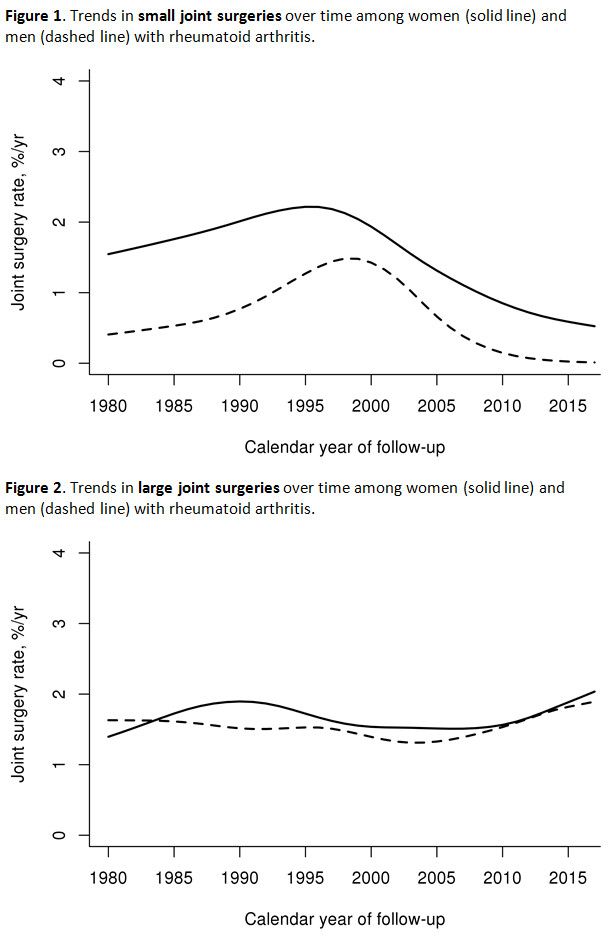
Results: The study included 739 women and 338 men with RA (mean age at incidence (±SD) 55.9±15.6 years). During a median follow up of 10.7 years, 90 women and 22 men underwent at least one small joint surgery (SJS) and 141 women and 63 men underwent at least one large joint surgery (LJS). The cumulative incidence of SJS was significantly higher in women (14.4% by 15 years after RA incidence; 95% confidence interval [CI}: 11.3-17.4%) than men (7.6% at 15 years; 95% CI: 4.3-10.8%; p=0.008), but no sex differences were noted in the cumulative incidence of LJS (20.2% at 15 years among women; 95% CI: 16.8-23.6% and 18.8% among men; 95% CI: 13.8-23.5%; p=0.55). The rates of small joint surgery declined in both sexes from 2000 onward (Figure 1; p=0.002), with no differences in trends between women and men (p=0.73). LJS rates were similar among both sexes (Figure2; p=0.85) and there was no evidence of a trend over time among both sexes combined (p=0.87).
Conclusion: Women with RA had a higher rate of SJS compared to men, although there is a declining trend in SJS rates over time in both sexes. There were no sex differences in rates of LJS, which is in contrast to higher rates of hip and knee arthroplasties seen in women compared to men in the general population1,2. This study also confirmed an absence of increase in rates of LJS among patients with RA during the study period.
References:
1. Kremers HM, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg. 2015;97:1386–97.
2. Singh JA, Vessely MB, Harmsen WS, et al. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969 to 2008. Mayo Clin Proc 2010;85:898–904.
To cite this abstract in AMA style:
Richter M, Crowson CS, Matteson EL, Makol A. Sex Differences in Orthopedic Surgery Among Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/sex-differences-in-orthopedic-surgery-among-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-differences-in-orthopedic-surgery-among-patients-with-rheumatoid-arthritis/