Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have an increased burden of multimorbidity. Although many comorbidities may vary by sex and men with lupus may have more severe disease than women, sex differences in multimorbidity among SLE patients have not been examined.
Methods: We used the OptumLabs Data Warehouse (OLDW), a longitudinal, real-world data asset with de-identified administrative claims for commercial and Medicare Advantage enrollees, to identify cases of SLE and matched comparators. Cases were defined as patients with ≥3 diagnoses of SLE between January 2006 and September 2015. Controls were persons without SLE matched 1:1 to SLE cases on age, sex, race/ethnicity, and enrollment date. Race was classified as non-Hispanic White (White), non-Hispanic Black (Black), Asian, Hispanic, based on self-report or derived rule sets. Multimorbidity (2 or more comorbidities) was defined using 172 chronic comorbidities from the chronic condition indicator of the clinical classification software (healthcare cost and utilization project). SLE, cutaneous lupus, and rheumatoid arthritis ICD-9 codes were excluded from the analysis. Two or more ICD-9 codes at least 30 days apart were used to define a comorbidity. A secondary analysis was performed including those with 5 or more comorbidities. Logistic regression models were used to estimate odds ratios (OR) with 95% confidence intervals (CI) adjusted for age, race/ethnicity, and region.
Results: The study included 34,752 cases with SLE and 34,752 matched non-SLE comparators. The mean age was 48 years (SD 14.2), and 90.6% were female for both cohorts in both cohorts, women were slightly younger (mean age 48 vs. 50 years). In both cohorts, women were more racially/ethnically diverse than men, with 66.2% of women (69.4% men) being White, 11.8% (12.3%) Hispanic, 18.7% (14.8%) Black, 3.4% (3.5%) Asian.
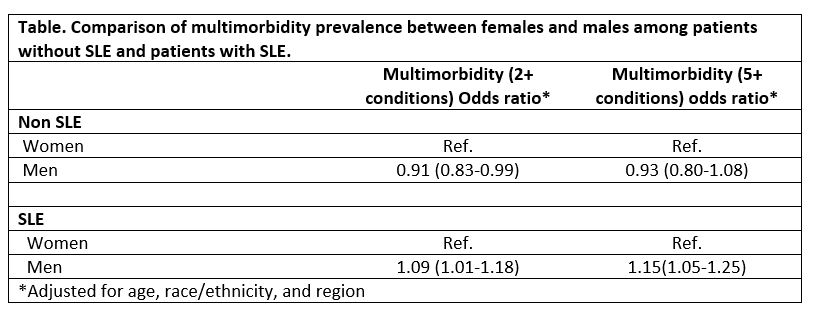
Patients with SLE had more multimorbidity than non-SLE subjects (58.1% vs 26.3%). Observed rates of multimorbidity were higher in men than women with SLE (57.8% women vs 60.9% men, p=0.0006), but similar non-SLE patients, (26.3% women vs 26.1% men, p=0.74). Following adjustment for age, race/ethnicity, and geographic region, multimorbidity among SLE patients remained higher in men (OR: 1.09; 95% CI: 1.01-1.18) compared to women and but lower for non-SLE men than women (OR: 0.91; 95% CI: 0.83-0.99). Secondary analysis in those with 5 or more comorbidities also demonstrated higher multimorbidity in men with SLE compared to women (OR: 1.15; 95%CI: 1.05-1.25), but similar in those without SLE (OR:0.93, 95% CI: 0.93 (0.8-1.08) (Table).
Conclusion: This large, nationwide claims study showed increased occurrence of multimorbidity in men with SLE compared to women with SLE, but similar to men and women without SLE. These differences may reflect the long-term effects of more severe disease in men with SLE than women.
To cite this abstract in AMA style:
Duarte-Garcia A, Heien H, Shah N, Crowson C. Sex Differences in Multimorbidity Between Patients with Systemic Lupus Erythematosus and Comparators in a Large Nationwide US Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/sex-differences-in-multimorbidity-between-patients-with-systemic-lupus-erythematosus-and-comparators-in-a-large-nationwide-us-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-differences-in-multimorbidity-between-patients-with-systemic-lupus-erythematosus-and-comparators-in-a-large-nationwide-us-study/