Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The extent to which heterogeneity exists in youth with axial disease and juvenile spondyloarthritis (JSpA) is unclear. In a cross-sectional sample of patients classified as axial disease in JSpA (axJSpA) according to recently validated criteria, we tested for differences in clinical and imaging features amongst males and females.
Methods: This was an international cross-sectional study of youth that met the following criteria: 1) Physician diagnosis of JSpA, 2) Symptom onset prior to age 18 years, 3) Fulfilled criteria for axJSpA. Clinical and magnetic resonance imaging (MRI) data were available from the time when axial disease was first identified; these features were compared between males and females using Pearson’s chi-squared and Fisher’s exact tests for categorical variables, and Wilcoxon rank-sum tests for continuous variables as appropriate. Multivariate logistic regression was used to assess the association of unequivocal inflammatory and structural lesions typical of axial disease on MRI and sex adjusted for HLA-B27 status and degree of inflammatory marker elevation.
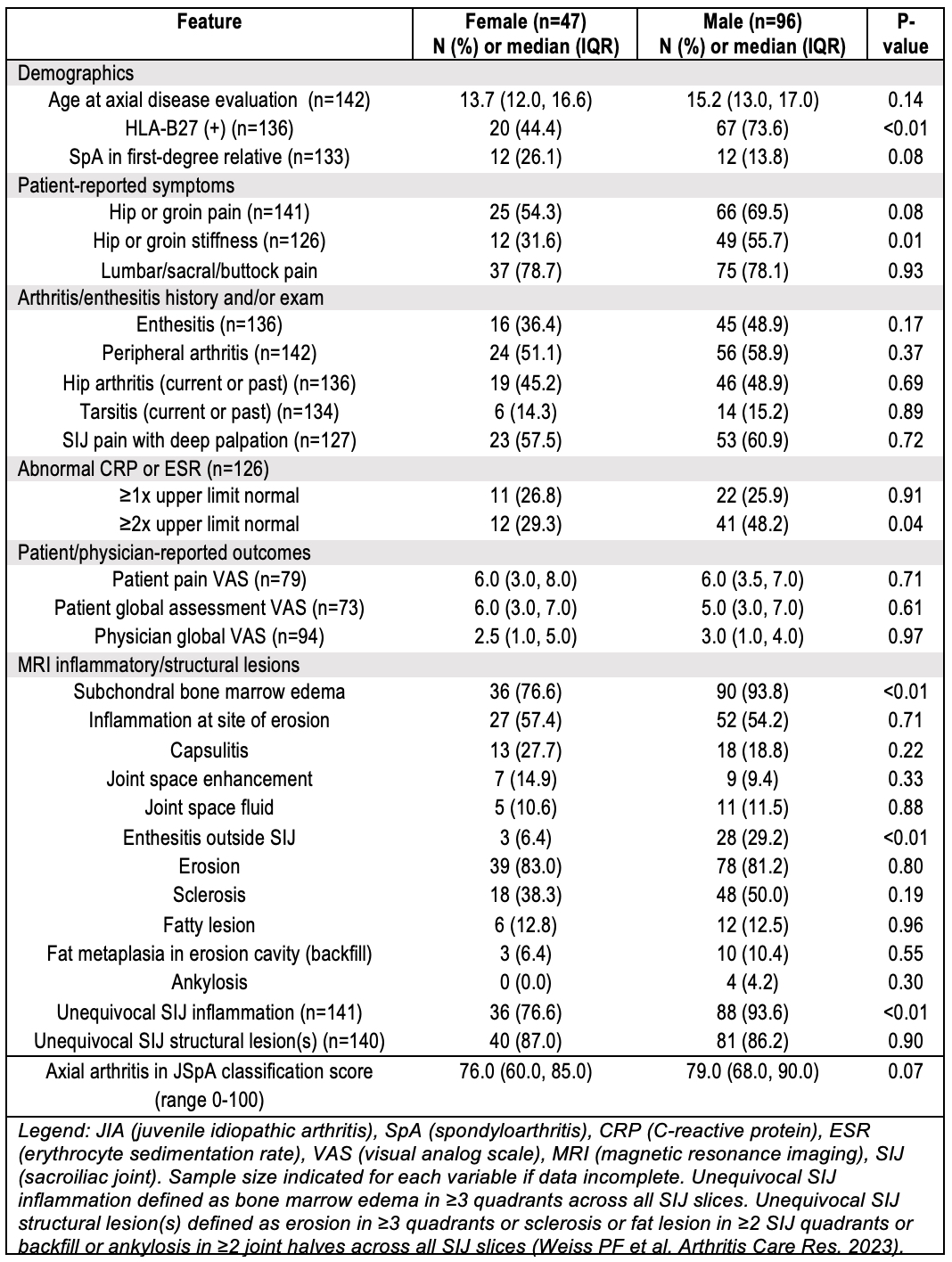
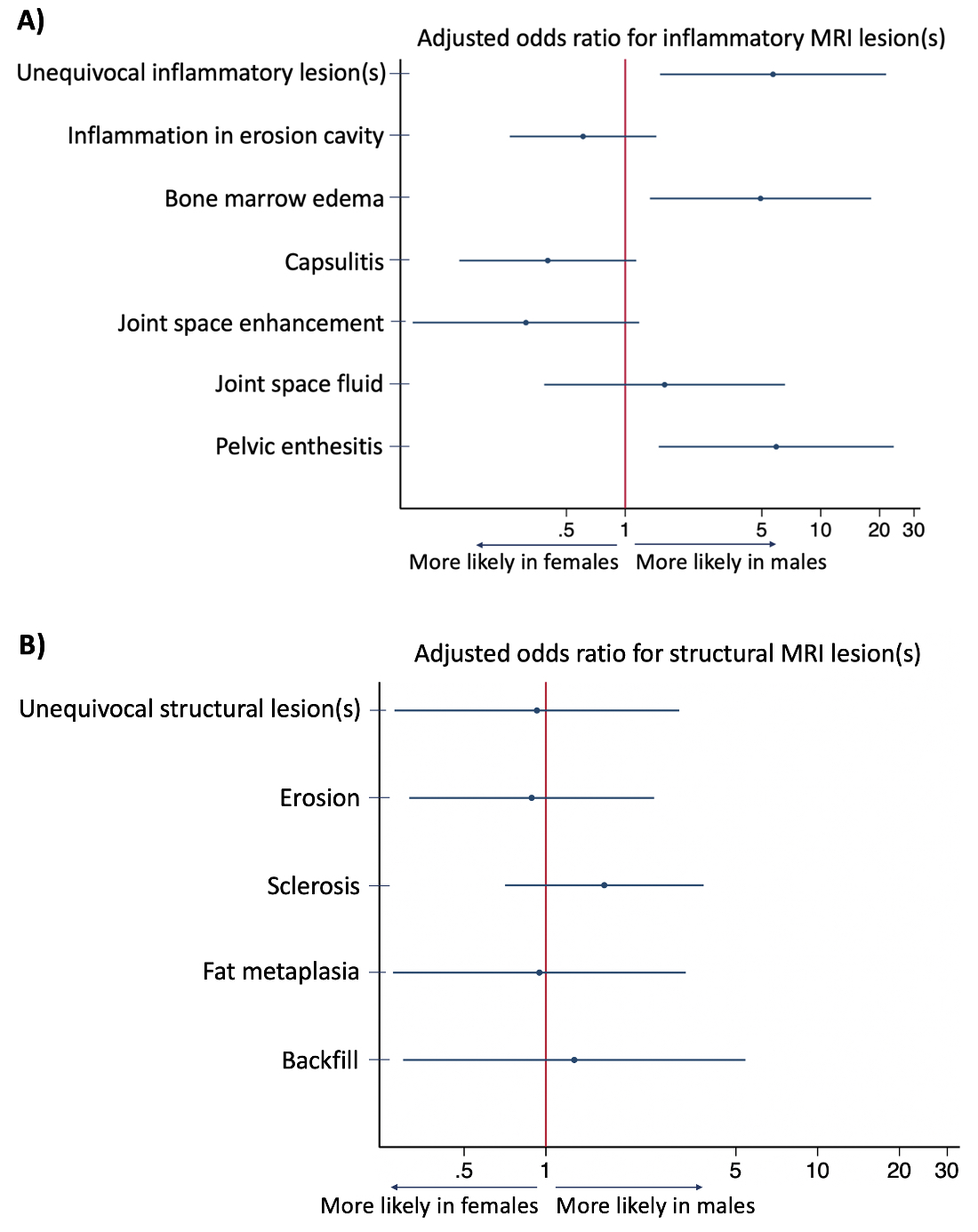
Results: 143 patients met inclusion criteria of which 96 (67.1%) were male, 64.0% were HLA-B27 positive, and 18.1% had a family history of spondyloarthritis in a first degree relative. Clinical and imaging characteristics stratified by sex are displayed in Table 1. Male patients had significantly greater prevalence of HLA-B27 positivity (p< 0.01), hip/groin stiffness (p=0.01), inflammatory markers ≥2x the upper limit of normal (p=0.04), pelvic enthesitis (p< 0.01), subchondral bone marrow edema (p< 0.01), and unequivocal sacroiliac joint inflammation on MRI (p< 0.01). There were no statistically significant differences between males and females in peripheral disease manifestations (current or history of) or patient-reported measures. After adjusting for HLA-B27 status and degree of inflammatory marker elevation, the odds of unequivocal inflammatory lesions typical of axial disease (OR 5.70, 95% CI 1.51-21.59), pelvic enthesitis outside the sacroiliac joint (OR 5.92, 95% CI 1.48-23.61) and subchondral bone marrow edema (OR 4.92, 95% CI 1.38-18.12) remained significantly higher in males (Figure 1A) but there were no differences between sexes with respect to structural MRI lesions (Figure 1B). The median axial disease classification score (range 0-100, classification threshold ≥55) was not significantly higher in males.
Conclusion: In patients with JSpA who met validated criteria for axJSpA the prevalence of HLA-B27 positivity, and serologic and imaging evidence of inflammation were significantly higher in males than females. Further exploration of the mechanisms underlying these differences is warranted, but our findings suggest that stratification by sex should be considered in the design of future studies in axJSpA.
To cite this abstract in AMA style:
Mayer A, Brandon T, Weiss P, JAXSPERT members o. Sex Differences in Clinical and Imaging Characteristics of Axial Juvenile Spondyloarthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/sex-differences-in-clinical-and-imaging-characteristics-of-axial-juvenile-spondyloarthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-differences-in-clinical-and-imaging-characteristics-of-axial-juvenile-spondyloarthritis/